Atherosclerosis is a condition that impacts millions of people worldwide, often silently, as it develops over decades without obvious symptoms. It’s a disease that lies at the heart of many of the world’s most significant health issues, including heart attacks, strokes, and peripheral artery disease. But what exactly is atherosclerosis? What causes it, and how does it affect the body in ways that can be life-threatening? To understand this complex and critical condition, we must first explore the inner workings of our arteries, the buildup of plaque, and how it leads to devastating consequences.
What Are Arteries, and Why Are They So Important?
To truly grasp the significance of atherosclerosis, we first need to understand the vital role arteries play in the circulatory system. Arteries are blood vessels responsible for carrying oxygen-rich blood from the heart to the rest of the body. These vessels are designed to handle high-pressure blood flow and are equipped with thick, elastic walls that allow them to expand and contract with each heartbeat.
The circulatory system is an intricate network, where arteries transport nutrients, oxygen, and hormones that are crucial for the health of tissues and organs. However, just as with any complex system, the arteries can face challenges that, over time, may compromise their function. One such challenge is the slow and gradual buildup of fatty substances, cholesterol, cellular waste products, and other debris within the artery walls—a process known as atherosclerosis.
The Origins of Plaque: The Building Blocks of Atherosclerosis
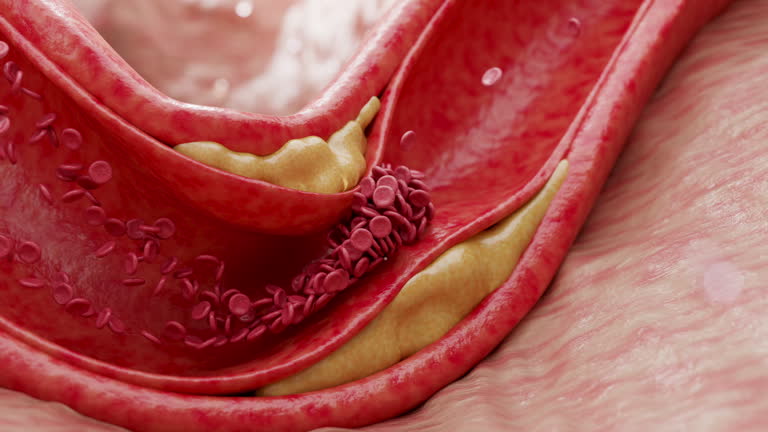
At the heart of atherosclerosis is the formation of plaque—often compared to rust building up on a pipe. Plaque is primarily composed of fat, cholesterol, and other cellular debris that accumulate within the walls of arteries. Initially, this buildup might not cause any immediate problems, but over time, it can thicken and narrow the arteries, making it more difficult for blood to flow through.
But what triggers this plaque buildup in the first place? The process begins when the lining of the arteries, known as the endothelium, becomes damaged. This can be caused by a number of factors, including high blood pressure, smoking, high cholesterol levels, or even chronic inflammation. The damaged endothelium becomes more permeable, allowing harmful substances like LDL (low-density lipoprotein) cholesterol, often referred to as “bad cholesterol,” to infiltrate the artery walls.
In response, the body sends white blood cells called macrophages to the site of damage. These cells attempt to digest the cholesterol and other debris. However, the process isn’t always effective. As the plaque continues to accumulate, it can harden over time, leading to further narrowing of the arteries. This condition is referred to as atherosclerosis.
The Role of Cholesterol in Plaque Formation
Cholesterol is a key player in the development of atherosclerosis, and understanding its role is crucial. Cholesterol itself is not inherently bad—our bodies actually need it to build cell membranes and produce hormones. However, the type of cholesterol and the levels in which it circulates in the bloodstream can have a significant impact on the risk of atherosclerosis.
There are two main types of cholesterol: LDL (low-density lipoprotein) and HDL (high-density lipoprotein). LDL cholesterol is often called “bad cholesterol” because it contributes to plaque buildup when it oxidizes and sticks to the artery walls. On the other hand, HDL cholesterol is often referred to as “good cholesterol” because it helps remove excess cholesterol from the bloodstream and transport it to the liver, where it can be processed and eliminated from the body.
When there is an imbalance—too much LDL cholesterol and not enough HDL cholesterol—plaque buildup in the arteries becomes more likely. High levels of LDL, combined with factors such as high blood pressure and smoking, make the arteries more vulnerable to damage. This is why doctors emphasize maintaining healthy cholesterol levels through diet, exercise, and, when necessary, medication.
The Stages of Atherosclerosis: From Fatty Streaks to Plaque Rupture
The development of atherosclerosis is not an overnight event; it’s a slow and gradual process that can take years, even decades, to unfold. The earliest stage of atherosclerosis is the formation of fatty streaks. These streaks consist primarily of small amounts of cholesterol that have accumulated in the artery walls. At this stage, the arteries still appear to function normally, and there are no visible symptoms.
As time passes, these fatty streaks can grow larger and evolve into plaques. This is when atherosclerosis becomes more dangerous. Plaques are made up of cholesterol, fat, calcium, and cellular debris. They protrude into the artery, narrowing the space through which blood can flow. As a result, blood flow becomes more restricted, and the heart has to work harder to pump blood through the narrower passages. This is the stage at which people may begin to experience symptoms, though they can still be subtle.
If the plaque continues to grow, it can rupture or break open, triggering the formation of a blood clot. This clot can block the artery completely, cutting off the blood supply to vital organs such as the heart or brain. If a clot forms in a coronary artery, it can result in a heart attack; if it forms in an artery leading to the brain, it can cause a stroke.
The Symptoms of Atherosclerosis: A Silent Threat
One of the most troubling aspects of atherosclerosis is its tendency to remain asymptomatic until it has progressed significantly. Many people with the condition may not know they have it until they experience a heart attack or stroke—events that often come as a complete surprise.
When symptoms do manifest, they can vary depending on which arteries are affected. If atherosclerosis develops in the coronary arteries (the blood vessels supplying the heart), it can lead to angina, a type of chest pain that occurs when the heart’s oxygen supply is insufficient. In severe cases, the buildup of plaque in the coronary arteries can lead to a heart attack.
If the carotid arteries (which supply blood to the brain) are affected, it can increase the risk of stroke. A transient ischemic attack (TIA), often referred to as a “mini-stroke,” may occur as a warning sign. This is characterized by sudden weakness, numbness, or vision changes, usually on one side of the body. While the symptoms of a TIA may be temporary, they indicate a serious underlying problem and should never be ignored.
In peripheral artery disease (PAD), atherosclerosis affects the arteries in the legs, leading to pain or cramping in the legs while walking. This is due to reduced blood flow to the muscles, which are in need of oxygen during physical activity. PAD is a common condition in people with atherosclerosis and can lead to more severe complications if left untreated.
Risk Factors: Who Is Most at Risk?
While atherosclerosis can affect anyone, certain factors significantly increase the risk of developing the condition. These include:
- Age: The risk of atherosclerosis increases with age, as the arteries naturally become stiffer and more prone to damage over time.
- Gender: Men are more likely to develop atherosclerosis at an earlier age, though the risk for women increases after menopause.
- Family History: A family history of heart disease or stroke can increase the likelihood of developing atherosclerosis.
- Chronic Conditions: High blood pressure, high cholesterol, diabetes, and obesity all contribute to the development of atherosclerosis.
- Lifestyle Factors: Smoking, lack of physical activity, and poor diet (particularly one high in saturated fats and sugars) significantly increase the risk.
- Excessive Alcohol Consumption: Drinking too much alcohol can raise blood pressure and increase the likelihood of atherosclerosis.
While these risk factors are important, the good news is that many of them can be controlled or managed with lifestyle changes, medication, and regular medical checkups.
Diagnosis: How Do Doctors Detect Atherosclerosis?
Because atherosclerosis is often asymptomatic in its early stages, diagnosing it can be challenging. However, several tests can help doctors detect the condition before it leads to a heart attack or stroke.
One of the most common tests is the lipid profile, which measures the levels of LDL cholesterol, HDL cholesterol, and total cholesterol in the blood. Elevated levels of LDL cholesterol and low levels of HDL cholesterol are strong indicators of atherosclerosis.
Other tests include:
- Blood Pressure Measurement: High blood pressure is a major risk factor for atherosclerosis, so regularly monitoring blood pressure is an important diagnostic tool.
- Electrocardiogram (ECG): An ECG can help detect heart abnormalities that might be related to atherosclerosis.
- Stress Testing: A stress test involves monitoring the heart’s response to exercise, which can reveal areas of the heart that are not receiving enough blood.
- Imaging Tests: Tests such as an ultrasound, CT scan, or MRI can create images of the blood vessels and help detect plaque buildup or blockages.
Treatment: Managing and Reversing Atherosclerosis
The treatment of atherosclerosis focuses on slowing or stopping the progression of plaque buildup and reducing the risk of complications like heart attacks and strokes. Early diagnosis and intervention are key to managing the condition effectively.
Treatment options include:
- Lifestyle Changes: A healthy diet, regular physical activity, smoking cessation, and weight management are foundational to managing atherosclerosis.
- Medications: Statins, blood pressure medications, and blood thinners are commonly prescribed to manage cholesterol levels, lower blood pressure, and reduce the risk of blood clots.
- Surgical Interventions: In severe cases of atherosclerosis, procedures like angioplasty (the insertion of a balloon to widen narrowed arteries) or coronary artery bypass surgery (CABG) may be necessary to restore blood flow.
Living with Atherosclerosis: A Path Forward
Atherosclerosis is a condition that demands attention, but it is also one that can be managed with the right approach. By understanding its causes, recognizing its symptoms, and taking proactive steps to reduce risk, it is possible to live a full and healthy life. Awareness, early intervention, and lifestyle changes are powerful tools in the fight against this “silent” disease.