In the grand saga of human survival, few inventions have had as dramatic an impact as antibiotics. These tiny molecular machines—often invisible, always potent—ushered in a golden age of medicine that many of us now take for granted. Imagine a world where a simple scratch could lead to death, where pneumonia was almost always fatal, and where surgical procedures often led to deadly infections. This was life before antibiotics.
Antibiotics didn’t just save lives; they reshaped the landscape of healthcare, expanded life expectancy, and made possible nearly every medical advancement of the 20th and 21st centuries. From organ transplants to chemotherapy, from safe childbirth to routine surgeries, none would be as safe—or even feasible—without these powerful drugs. But what exactly are antibiotics? How do they work? Where do they come from? And why is the world suddenly worried about antibiotic resistance?
In this article, we journey deep into the fascinating world of antibiotics: from their accidental discovery and biological mechanisms to the urgent threats they now face.
A Brief History: Mold, Chance, and Genius
The story of antibiotics begins with an accident. In 1928, Scottish bacteriologist Alexander Fleming returned from a vacation to find something strange in one of his petri dishes. A mold—later identified as Penicillium notatum—was preventing the growth of Staphylococcus bacteria. The mold had produced a substance that killed bacteria. Fleming named it penicillin.
Though his discovery was revolutionary, the journey from petri dish to pharmacy shelf was slow. It wasn’t until World War II, when scientists like Howard Florey, Ernst Chain, and Norman Heatley found ways to mass-produce penicillin, that antibiotics truly entered the global stage. The timing was fortuitous. As soldiers were falling not only to bullets but to infections, penicillin became a miracle cure. The Allies mass-produced it, saving thousands of lives and changing the course of the war—and medicine.
Following penicillin’s success, pharmaceutical companies and researchers raced to discover more antibiotics. Streptomycin, tetracycline, erythromycin, and others followed, each targeting different types of bacteria. The golden era of antibiotic discovery had begun.
What Are Antibiotics?
At their core, antibiotics are chemical substances designed to combat bacterial infections. Unlike antiviral drugs, which target viruses, or antifungals, which treat fungal infections, antibiotics specifically work against bacteria—organisms that are alive, single-celled, and can reproduce independently.
Antibiotics can be natural (produced by fungi or bacteria to outcompete rivals), semi-synthetic (modified from natural compounds), or synthetic (designed entirely in the lab). Their purpose? To either kill bacteria outright (bactericidal) or stop them from reproducing (bacteriostatic).
But here’s the truly fascinating part: antibiotics exploit the biological differences between human cells and bacterial cells. This is what allows them to fight infection without harming the host (most of the time). Understanding how antibiotics differentiate between “us” and “them” is key to appreciating their elegant mechanism.
How Do Antibiotics Work?
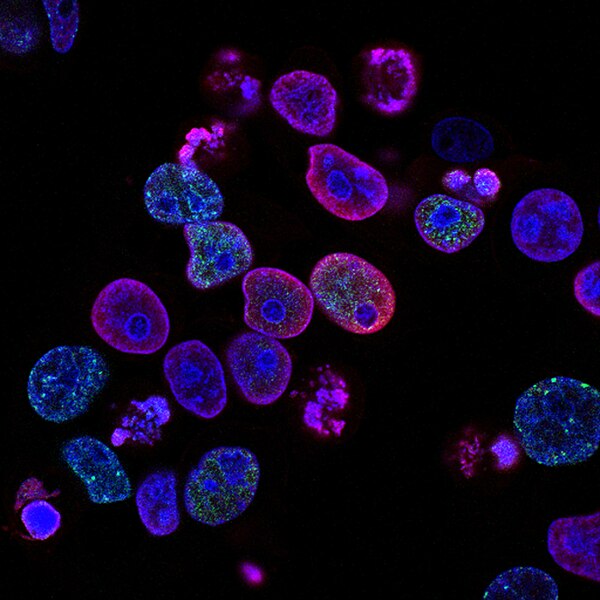
To appreciate how antibiotics work, you need to understand the target: the bacterial cell. Bacteria differ from human cells in several critical ways, and antibiotics exploit those differences in several clever manners.
Some antibiotics, like penicillin, attack the bacterial cell wall. Human cells don’t have cell walls, so penicillin and its relatives can disable bacteria without harming human tissue. Penicillin weakens the wall, causing the bacteria to burst under pressure.
Others, like tetracycline and erythromycin, disrupt bacterial protein synthesis. They latch onto bacterial ribosomes—the cellular machines that assemble proteins—and jam the gears. Because bacterial ribosomes are structurally different from human ones, these antibiotics can interfere with bacterial growth without affecting our own cells.
Then there are antibiotics like ciprofloxacin that attack bacterial DNA replication. They prevent the bacteria from reproducing, effectively sterilizing them.
And some, like sulfonamides, mimic bacterial nutrients and slip into their metabolic machinery, sabotaging their essential processes from within.
Each class of antibiotic has its specialty, and doctors choose them based on the nature of the infection, the bacteria involved, and the patient’s health.
Types of Antibiotics: One Size Doesn’t Fit All
Not all antibiotics are created equal. Some are narrow-spectrum, targeting specific types of bacteria—say, only gram-positive organisms (those with thick cell walls). Others are broad-spectrum, capable of tackling a wide array of bacteria, including both gram-positive and gram-negative strains.
Penicillin, for instance, is more effective against gram-positive bacteria like Streptococcus and Staphylococcus. Ciprofloxacin, on the other hand, can take on a broader range of bacteria, making it useful for more complex infections.
Doctors must walk a fine line when prescribing antibiotics. A narrow-spectrum antibiotic is ideal because it minimizes damage to the body’s beneficial bacteria—our microbiome. But when the exact culprit isn’t known, broad-spectrum antibiotics may be necessary. Unfortunately, this practice contributes to a major modern crisis: antibiotic resistance.
Antibiotics and the Microbiome: Friends, Foes, and Fallout
Our bodies are home to trillions of bacteria—most of them friendly or benign. They live on our skin, in our guts, and throughout our bodies, helping digest food, synthesize vitamins, and regulate our immune systems. This ecosystem is called the microbiome, and it’s vital to our health.
When we take antibiotics, especially broad-spectrum ones, we risk disturbing this delicate balance. While the drug fights the infection, it also wipes out helpful bacteria. This can lead to side effects like diarrhea, yeast infections, or more serious problems like Clostridioides difficile overgrowth, which can cause life-threatening colitis.
There’s growing evidence that repeated antibiotic use, especially in early childhood, may have long-term consequences. It can alter the microbiome in ways that affect metabolism, immunity, even brain development. Scientists are only beginning to understand these effects, but the message is clear: antibiotics, while lifesaving, must be used with care.
The Looming Threat of Antibiotic Resistance
Here lies the dark side of antibiotics: their incredible success has led to overuse, misuse, and a global crisis. Bacteria are evolutionary geniuses. Under the pressure of antibiotic assault, they adapt. They mutate. They evolve.
Some bacteria acquire resistance genes through random mutation. Others “borrow” resistance genes from neighboring microbes through horizontal gene transfer—a sort of microbial knowledge exchange. Over time, these resistant strains survive, thrive, and spread.
The result? Infections that were once easily treatable are now becoming deadly again. Diseases like tuberculosis, gonorrhea, and urinary tract infections are growing increasingly resistant. Hospital-acquired infections caused by superbugs like MRSA (Methicillin-resistant Staphylococcus aureus) and CRE (Carbapenem-resistant Enterobacteriaceae) kill thousands each year.
According to the World Health Organization, antibiotic resistance is one of the greatest threats to global health. If nothing changes, we could return to a pre-antibiotic era where routine surgeries and common infections become high-risk events.
Causes of Antibiotic Resistance: A Perfect Storm
The roots of resistance are complex but identifiable. Overprescription by doctors plays a major role. Too often, antibiotics are given for viral infections like the flu or common cold, against which they are powerless. In some countries, antibiotics are available over the counter, leading to unregulated usage.
Agriculture is another culprit. In many nations, antibiotics are used not just to treat sick animals, but to promote growth and prevent disease in healthy livestock. This creates a breeding ground for resistant bacteria, which can jump from animals to humans via food, water, or direct contact.
Incomplete courses of antibiotics also contribute. When patients stop treatment early—because they feel better or to “save” leftover pills—they leave behind surviving bacteria that are often the most resilient. These become the ancestors of future resistant strains.
The Global Response: Strategies to Combat Resistance
Fighting antibiotic resistance requires a multi-pronged approach. Education is vital. Patients need to understand that not all infections require antibiotics, and that finishing a prescribed course is essential.
Doctors are being trained to prescribe more judiciously. Rapid diagnostic tools are being developed to distinguish bacterial from viral infections, reducing unnecessary antibiotic use.
Hospitals are implementing stewardship programs to track and manage antibiotic use. Agricultural policies are shifting, banning the use of medically important antibiotics for growth promotion in animals.
Researchers are hunting for new antibiotics, though the pipeline has slowed in recent decades. Antibiotic development is expensive and scientifically challenging. But hope is not lost: new classes, like teixobactin, are emerging, and novel strategies—like bacteriophage therapy (using viruses that target bacteria)—are being explored.
Beyond Pills: The Future of Antibacterial Defense
While antibiotics remain essential, the future of infection control may include new tools. Scientists are studying antimicrobial peptides—tiny proteins produced by our own bodies that kill bacteria without breeding resistance.
CRISPR-based antimicrobials are in development, using genetic tools to selectively destroy resistant bacteria while sparing beneficial ones.
Probiotics and microbiome restoration therapies are being used to repair the damage caused by antibiotics, especially in the gut.
Vaccines may also play a larger role. By preventing bacterial infections in the first place, vaccines reduce the need for antibiotics. The pneumococcal vaccine, for example, has significantly decreased infections by Streptococcus pneumoniae, a major cause of pneumonia and meningitis.
Conclusion: Antibiotics as a Double-Edged Sword
Antibiotics are among the greatest achievements in medical history. They have saved hundreds of millions of lives, made modern medicine possible, and reshaped how we view infectious disease. But with great power comes great responsibility.
We now face a global crossroads. If we continue to overuse and misuse antibiotics, we risk plunging back into an era of untreatable infections. If, however, we treat these precious drugs with respect—using them only when necessary, completing courses, and supporting research—we can preserve their power for future generations.
Understanding antibiotics is not just for scientists and doctors. It’s for anyone who takes a pill, visits a hospital, or eats food. In short: it’s for everyone. Because these marvel molecules aren’t just part of our history—they are the guardians of our future.