Every moment of every day, a quiet war is waged within and around our bodies. It is invisible to the naked eye, yet its consequences have shaped the course of human history—toppling empires, altering populations, and sparking revolutions in science and medicine. This war is fought between the cells of our body and tiny invaders known as pathogens.
These infectious microbes—viruses, bacteria, fungi, and parasites—are not mindless, nor are they evil. They are simply following the imperative of life: to survive and reproduce. In doing so, some take advantage of us, their hosts, using our cells, fluids, and systems to grow and spread. When they cause harm in the process, we call them pathogens.
But what exactly are pathogens? How do they operate? Where do they come from, and how do they differ from the many harmless or even beneficial microbes that surround us? The answers to these questions reveal a fascinating, often startling world—one that is at once ancient, dynamic, and deeply intertwined with our own.
Microbes: Friends, Foes, and Everything In Between
Before we define pathogens, we must first appreciate the broader family to which they belong: microorganisms. These include bacteria, viruses, archaea, fungi, protozoa, and microscopic parasites. The vast majority of these microbes are not harmful. In fact, many are essential for life.
Inside your gut live trillions of bacteria that help digest food, regulate your immune system, and even influence your mood. On your skin, microbes form a protective barrier against invaders. In the soil, fungi and bacteria decompose organic matter and enrich ecosystems. Microbes were among the first forms of life on Earth and will likely outlast us.
Pathogens are a small, dangerous minority within this microbial universe. They are defined not by their size or structure, but by their relationship with us. A pathogen is any microbe that causes disease in its host. It is not always a black-and-white distinction; some microbes can be harmless in one context and pathogenic in another, depending on the health of the host or the location in the body.
This dynamic nature makes the study of pathogens not just a branch of microbiology, but a journey into ecology, evolution, and human vulnerability.
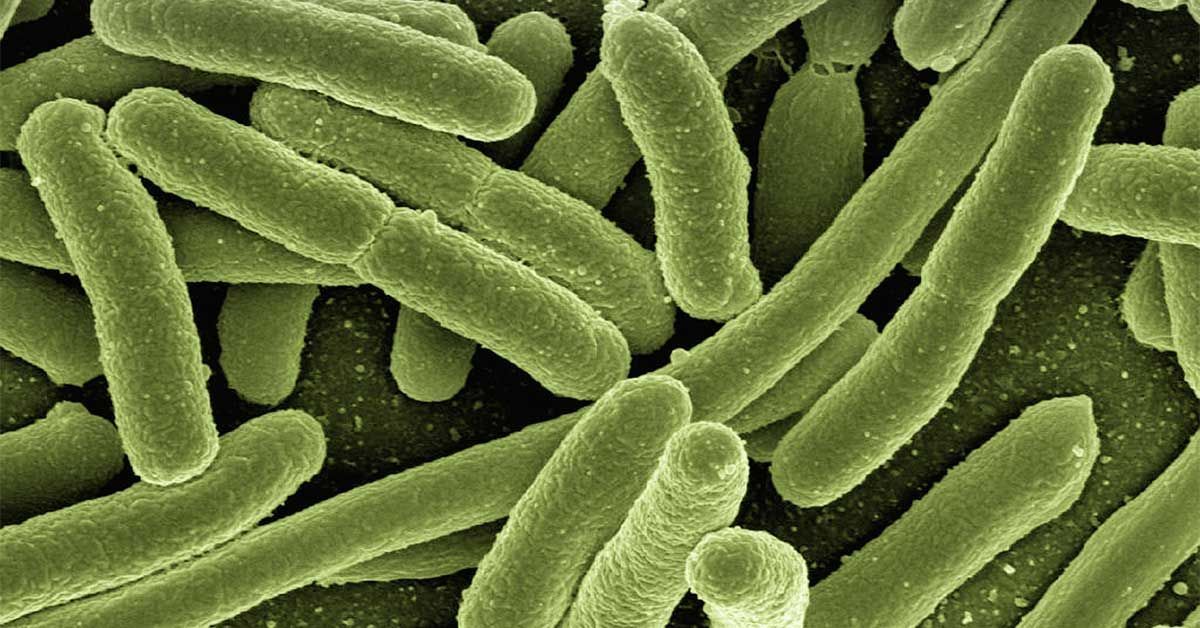
Bacteria: Ancient Invaders With Modern Impact
Bacteria are among the oldest and most versatile life forms on Earth. They are single-celled organisms that can thrive in extreme environments—from boiling hydrothermal vents to frozen tundras. Many bacteria are harmless or beneficial. But some have evolved mechanisms to invade our bodies and disrupt our systems.
Pathogenic bacteria cause illnesses ranging from the mild to the life-threatening. Streptococcus pyogenes causes strep throat and scarlet fever. Mycobacterium tuberculosis is the agent behind tuberculosis, which has killed more people than any other infectious disease in human history. Salmonella, E. coli, and Clostridium botulinum can cause severe foodborne illnesses.
These bacteria don’t simply float aimlessly into our bodies. They possess specialized tools—adhesins to stick to our tissues, toxins to break open cells, capsules to evade immune detection. Some bacteria, like Helicobacter pylori, even burrow into the protective mucus lining of the stomach, surviving an acidic hellscape to cause ulcers.
Antibiotics, discovered in the 20th century, revolutionized the treatment of bacterial infections. But overuse and misuse have fueled the rise of antibiotic-resistant strains, such as MRSA (methicillin-resistant Staphylococcus aureus), making bacterial pathogens a renewed global threat.
Viruses: The Ultimate Parasites
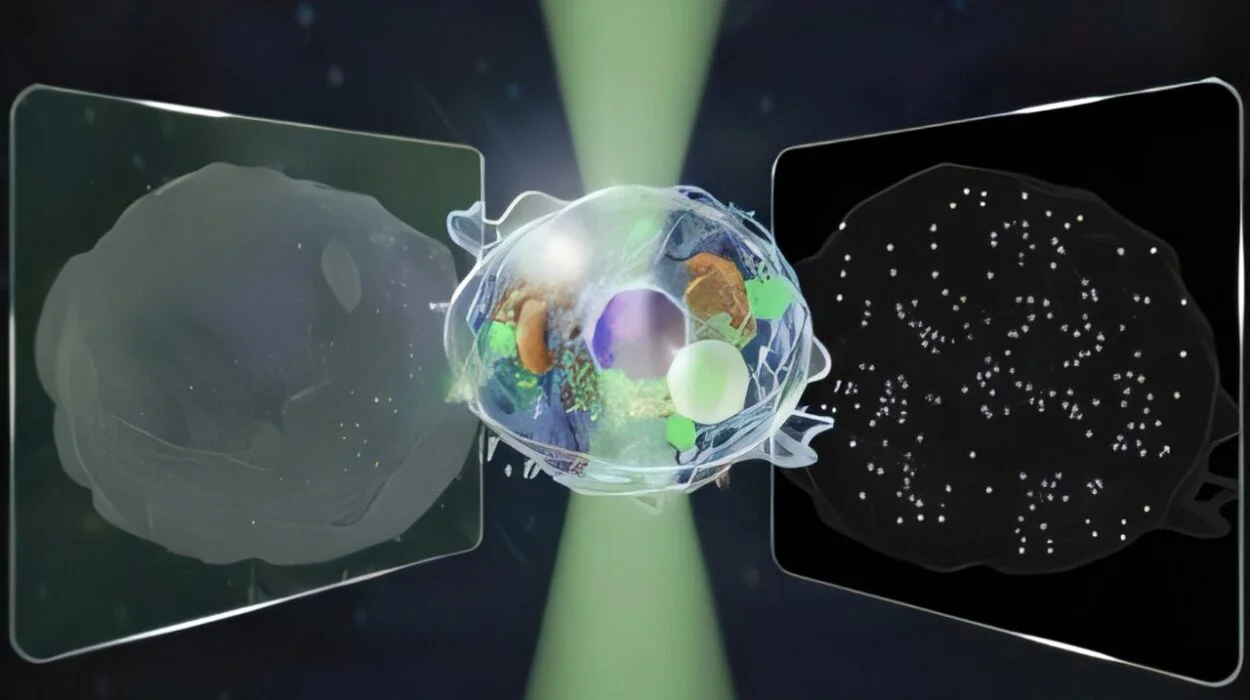
Viruses are perhaps the most enigmatic pathogens. They are not alive in the traditional sense—they cannot replicate on their own, eat, or carry out metabolic functions. Instead, they are genetic ghosts: mere strands of DNA or RNA wrapped in a protein shell. But once inside a living cell, they become ruthless hijackers.
A virus infects by injecting its genetic material into a host cell, reprogramming the cell to produce more copies of the virus. The cell becomes a virus factory—until it bursts, releasing new viral particles to infect neighboring cells. This simple yet devastating strategy underlies many of the world’s deadliest diseases: HIV/AIDS, influenza, COVID-19, hepatitis, measles, rabies.
Some viruses, like herpes simplex, lie dormant for years before reactivating. Others, such as Zika or Ebola, cause sudden, explosive outbreaks. Viruses can mutate rapidly, evade immune detection, and cross species barriers—jumping from animals to humans in so-called zoonotic events, often with tragic consequences.
Vaccines, more than any other intervention, have helped humanity push back against viral pathogens. From smallpox to polio to COVID-19, vaccines prime the immune system to recognize and neutralize viruses before they cause harm. Yet as the SARS-CoV-2 pandemic showed, viral evolution can outpace our defenses, demanding constant vigilance and innovation.
Fungi: Opportunistic and Occasionally Lethal
Fungi occupy a strange space in the pathogen landscape. While most are decomposers that break down organic material in forests and compost heaps, some can infect humans—especially when our immune defenses are weakened.
Fungal infections range from the superficial, like athlete’s foot or ringworm, to the deeply invasive. Candida albicans, a yeast that normally lives harmlessly in the body, can cause thrush or life-threatening systemic infections in immunocompromised individuals. Cryptococcus neoformans can cause deadly meningitis in people with HIV/AIDS. Aspergillus fumigatus, a mold found in decaying vegetation, can trigger allergic reactions or invade the lungs.
Unlike bacteria, fungi are eukaryotic—meaning their cells are more similar to ours. This makes them harder to target with drugs without harming human cells. Antifungal resistance is a growing concern, especially with the emergence of multidrug-resistant species like Candida auris, which can survive on hospital surfaces and cause outbreaks.
Fungi have a unique relationship with temperature. Most cannot grow at the high body temperatures of mammals. But climate change may be altering this barrier, allowing new fungal pathogens to emerge. The microbial line between environment and infection is blurring.
Parasites: Masters of Manipulation
Parasites are organisms that live in or on a host and derive nutrients at the host’s expense. Many are visible under a microscope—or even to the naked eye—and have complex life cycles involving multiple hosts. Parasitic pathogens are especially common in tropical and subtropical regions, where warm climates and poor sanitation facilitate transmission.
Some parasites, like Plasmodium falciparum, the agent of malaria, are protozoa—single-celled eukaryotes. Others, like Taenia solium (pork tapeworm) or Ascaris lumbricoides (giant roundworm), are helminths—multicellular worms that can grow to grotesque lengths inside the body. Still others, like Sarcoptes scabiei, are ectoparasites that live on the skin, causing scabies.
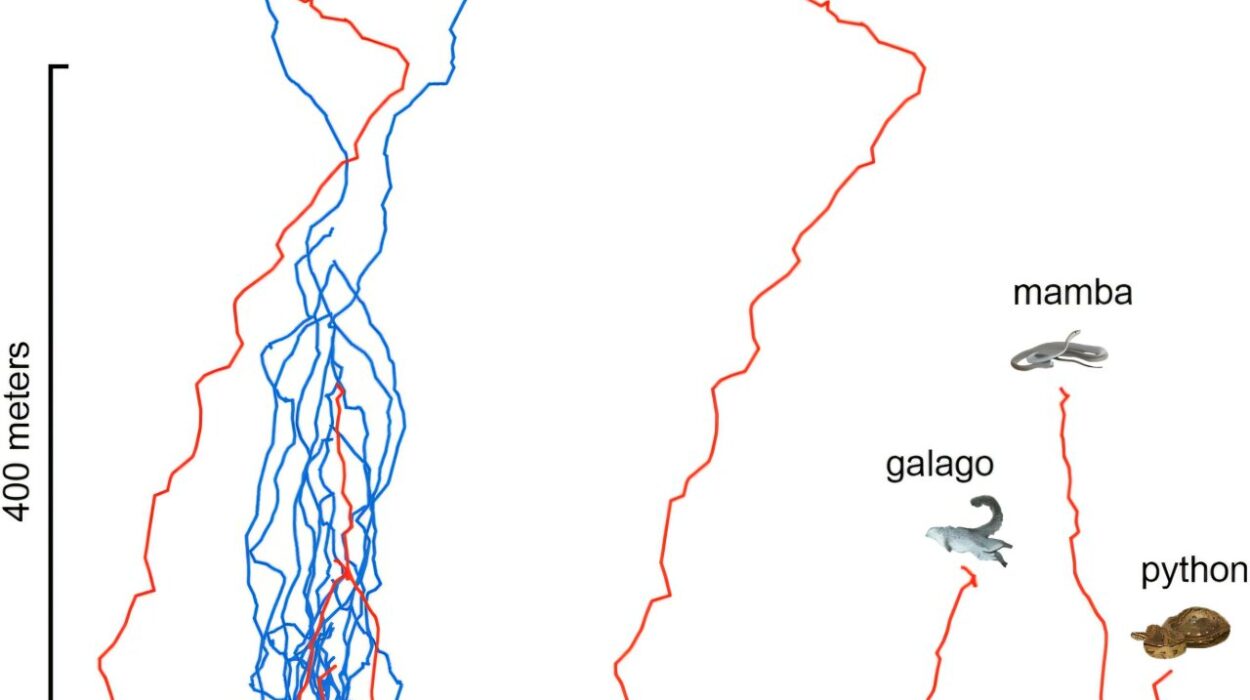
Parasites have evolved extraordinary survival strategies. Some mimic host molecules to avoid detection. Others manipulate host behavior, as Toxoplasma gondii may do in infected rodents and potentially humans. Many parasites cycle between hosts—mosquitoes, snails, flies—using them as vectors to complete their life stages.
Controlling parasitic diseases often requires a combination of drug treatment, vector control, improved sanitation, and education. Despite decades of effort, diseases like malaria, schistosomiasis, and leishmaniasis continue to affect hundreds of millions each year.
How Pathogens Cause Disease
Pathogenicity—the ability to cause disease—is not a fixed trait but a spectrum. Some microbes cause illness in almost everyone they infect. Others do so only under certain conditions: when the immune system is suppressed, the skin is broken, or the microbial balance is disrupted.
To cause disease, a pathogen must follow several steps. First, it must enter the host, often through the respiratory tract, gastrointestinal tract, skin wounds, or mucosal surfaces. Next, it must establish a foothold, overcoming innate defenses like stomach acid, enzymes, and immune cells. Then, it multiplies and spreads, releasing toxins or triggering damaging immune responses.
Finally, it must find a way to exit the host and infect others—via coughs, sneezes, blood, feces, urine, or sexual fluids. This cycle of transmission is what sustains the pathogen’s existence.
Disease symptoms are not always caused directly by the microbe. Sometimes they result from the immune system’s attempt to fight it. Fever, inflammation, fatigue—these can be signs of a battle underway. In other cases, pathogens release toxins that directly damage tissues, as in botulism or cholera.
Understanding these mechanisms allows scientists and doctors to intervene at different stages—blocking entry, boosting defenses, neutralizing toxins, or breaking chains of transmission.
The Immune System: Defender of the Realm
Our immune system is a marvel of biological engineering, honed by millions of years of coevolution with pathogens. It consists of two main arms: the innate immune system, which offers rapid but general defense, and the adaptive immune system, which mounts a targeted and memory-based response.
When a pathogen breaches our barriers, innate defenses like macrophages, neutrophils, and natural killer cells attack. They release chemical signals that trigger inflammation and summon reinforcements. If the threat persists, adaptive immunity kicks in. T-cells recognize infected cells and destroy them. B-cells produce antibodies that neutralize invaders.
Once a pathogen is defeated, the immune system often retains a memory, making future encounters less dangerous. This is the principle behind vaccination: training the immune system with a harmless version of the pathogen.
But not all immune responses are helpful. Sometimes, they overreact—causing allergies, autoimmune diseases, or sepsis. And some pathogens, like HIV, specifically target immune cells, dismantling the body’s defenses from within.
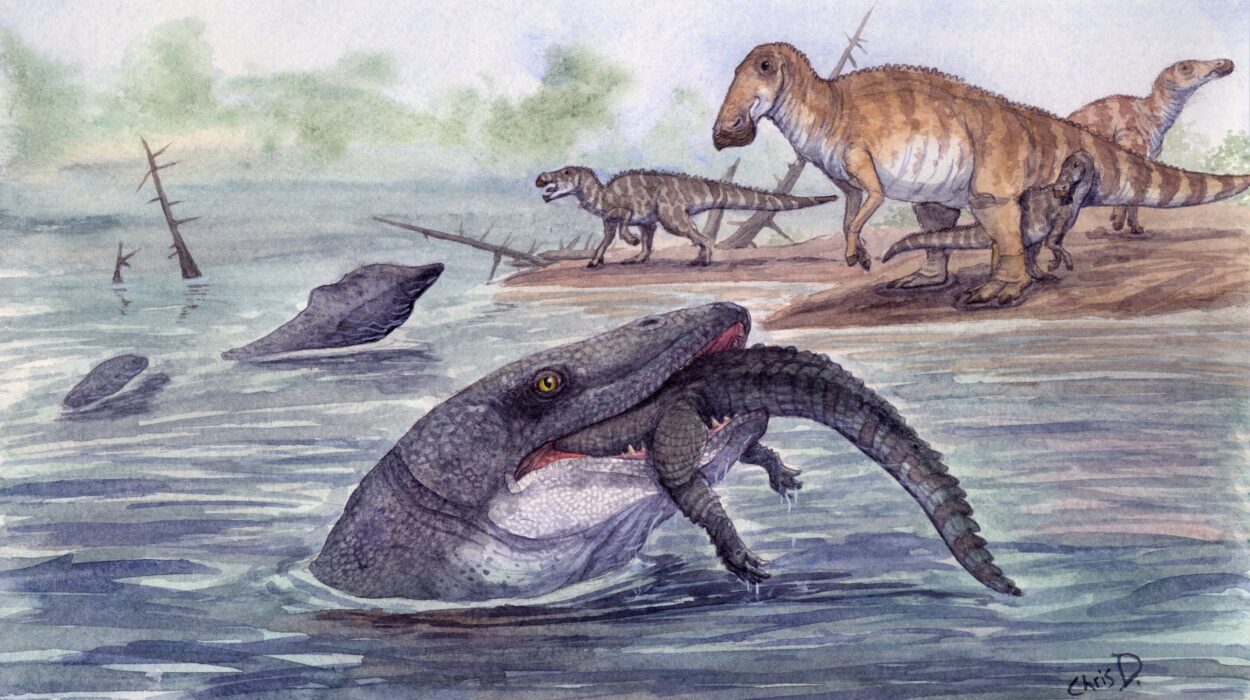
Zoonotic Spillover and Emerging Pathogens
Many of the most devastating infectious diseases in humans originated in animals. These zoonotic pathogens include HIV (from primates), influenza (from birds and pigs), Ebola (from bats), and coronaviruses like SARS, MERS, and COVID-19.
Zoonotic spillover occurs when a pathogen jumps from an animal host into humans, often due to environmental disruption, wildlife trade, or agricultural intensification. Forest clearing, for example, can bring humans into closer contact with bats and their viruses. Wet markets and exotic pet trade increase the risk of viral recombination and cross-species transmission.
Once inside a human host, the pathogen must adapt to our cells, replicate effectively, and spread between people. Most fail. But when one succeeds, the results can be catastrophic. The COVID-19 pandemic reminded the world how rapidly a novel virus can reshape global health, economies, and societies.
Monitoring animal reservoirs, enhancing surveillance, and investing in global health infrastructure are crucial for preventing the next pandemic. Pathogens do not recognize borders. Our response must be equally global.
Antibiotics, Antivirals, and Resistance
Modern medicine owes much of its power to antimicrobial agents: antibiotics for bacteria, antivirals for viruses, antifungals for fungi, and antiparasitics for worms and protozoa. These drugs target specific parts of the pathogen’s biology—cell walls, enzymes, replication machinery—disabling them while sparing human cells.
But microbes are not static. They evolve. Under pressure from drugs, they mutate and adapt. Resistance spreads through populations, rendering treatments ineffective. Multidrug-resistant tuberculosis, gonorrhea, and fungal infections are already major threats. Some bacteria now resist every antibiotic we have.
The overuse of antibiotics in medicine and agriculture accelerates this crisis. So does the lack of new drug development. Addressing antimicrobial resistance requires a global effort: better stewardship, faster diagnostics, novel therapies, and alternative approaches like phage therapy or CRISPR-based antivirals.
The Microbial Future
As we map the genomes of pathogens, track their evolution in real time, and explore the microbiome’s role in health, we are entering a new era of microbiology—one that transcends the simple dichotomy of friend or foe.
We now understand that pathogens evolve not in isolation, but in ecological contexts shaped by climate, society, and behavior. Urbanization, travel, poverty, conflict—all create fertile ground for outbreaks. At the same time, scientific advances offer hope: mRNA vaccines, real-time sequencing, AI-guided drug discovery.
The story of pathogens is not one of evil microbes attacking innocent hosts. It is a story of interaction, coevolution, and adaptation. We are not passive victims. We are active participants in a biological drama that spans millennia.
Conclusion: The Invisible Mirror
To understand pathogens is to understand ourselves—not just as organisms vulnerable to disease, but as beings embedded in a vast, unseen web of life. Pathogens test our defenses, yes—but they also reveal our ingenuity, our interconnectedness, and our responsibility to each other and the planet.
In every fever and recovery, every vaccine and outbreak, we glimpse the ongoing dialogue between human life and microbial life. It is a dialogue written in DNA, carried in blood and breath, and recorded in the pages of medical history.
We may never eliminate all pathogens. But with knowledge, empathy, and vigilance, we can learn to live with them—and protect the most precious gift they challenge: our health.