Imagine this: you’re not feeling well, and after a visit to your doctor, you’re handed a prescription. You take the medication with the expectation of relief and recovery. But then, your stomach starts to churn, or perhaps you feel unusually drowsy. Maybe a rash appears, or your mood shifts inexplicably. These are the shadows lurking behind the promises of modern medicine — the side effects.
Side effects are the uninvited guests of the healing process, the unpredictable companions of therapeutic interventions. While drugs are designed to help us, they often come with a catch — effects that were not the primary intention of treatment. Some are mild and barely noticeable, while others can be severe, even life-threatening.
Understanding side effects isn’t just for doctors or pharmacists. It’s essential knowledge for anyone who’s ever popped a pill, applied a cream, or received a vaccine. In this article, we’ll explore what side effects are, how they happen, why they vary so much from person to person, and what modern medicine is doing to manage or even eliminate them.
Defining Side Effects: More Than Just a Nuisance
In the simplest terms, a side effect is an unintended response to a medication or medical intervention. It’s a biological reaction that is not the desired therapeutic outcome. This doesn’t mean it’s always bad — in fact, some side effects are beneficial — but usually, the term carries a negative connotation.
Medically, side effects are sometimes referred to as “adverse effects,” especially when they are harmful. The broader medical term is “adverse drug reaction” (ADR), which includes both predictable and unpredictable reactions. Not all side effects are dangerous, but they can interfere with treatment, reduce patient compliance, or necessitate additional medications to counteract them.
Let’s say you’re taking an antihistamine for allergies. It stops your sneezing and itchy eyes — success! But now you feel groggy all day. That drowsiness is a side effect. It wasn’t the intended purpose, but it happened because of how the drug interacts with your body.
The Body Is Not a Machine: Complexity Breeds Variability
To understand why side effects happen, we need to delve into the nature of the human body and how drugs interact with it. Unlike a machine, the body is an incredibly complex and dynamic biological system. Each cell, organ, and enzyme plays a part in maintaining a delicate balance — and medications can disrupt that balance.
Drugs are essentially chemicals introduced into this living system. They are designed to interact with specific targets — receptors, enzymes, or tissues — to correct a problem. But no drug is completely selective. Most medications have multiple effects on the body, affecting not just the intended target but other systems as well.
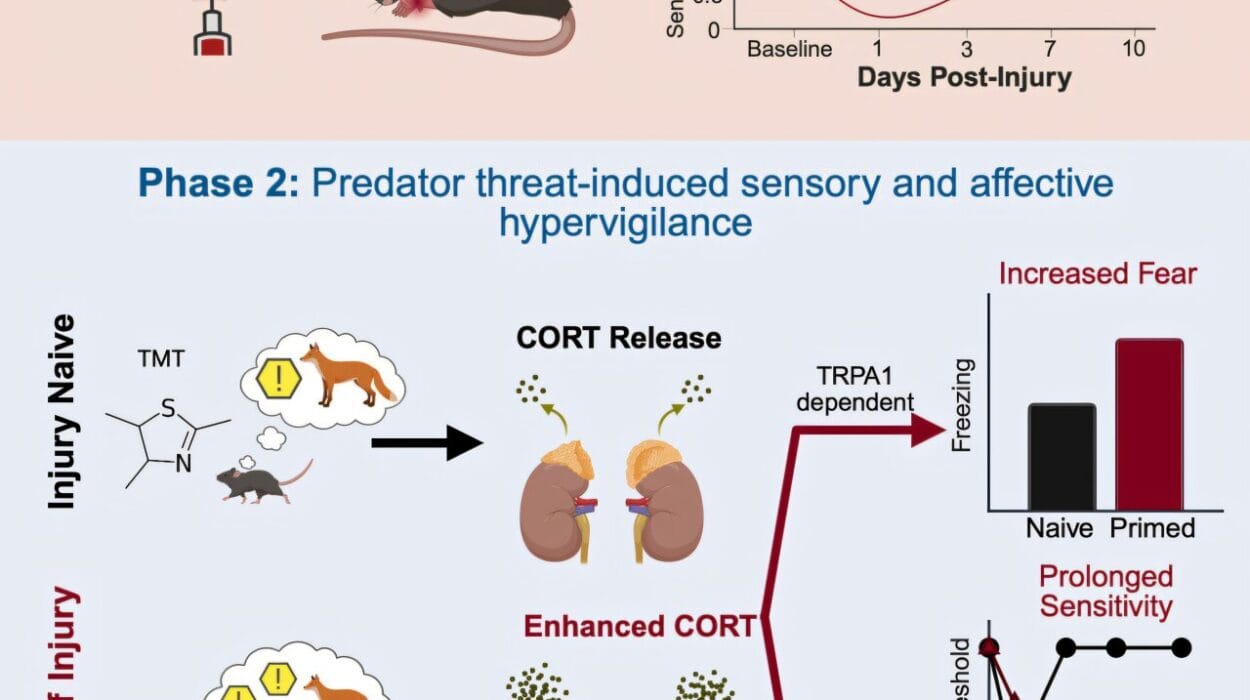
This off-target activity is where many side effects originate. The more widespread a drug’s action, the more likely it is to produce unintended consequences. Moreover, every individual’s biology is slightly different. Genetics, age, gender, weight, liver function, kidney efficiency, other medications, and even diet can all influence how a drug behaves in the body.
Imagine throwing a stone into a calm pond. The splash might hit a specific point, but the ripples spread far and wide. Similarly, a drug might aim at one process but ends up influencing many others.
The Pharmacokinetics and Pharmacodynamics of Side Effects
To truly grasp side effects, we must understand two key concepts in pharmacology: pharmacokinetics and pharmacodynamics.
Pharmacokinetics refers to what the body does to a drug. It includes absorption (how a drug enters the bloodstream), distribution (how it spreads through the body), metabolism (how it is broken down), and excretion (how it leaves the body). If any of these processes go awry — for instance, if the liver doesn’t metabolize the drug efficiently — the drug may linger too long, accumulate to toxic levels, or be ineffective.
Pharmacodynamics, on the other hand, deals with what the drug does to the body. It looks at the biochemical and physiological effects and how the drug interacts with its target. Side effects can arise from the drug binding to unintended receptors or affecting non-target tissues.
Take beta-blockers, for example. These are used to manage high blood pressure by slowing the heart rate. But they can also cause fatigue or cold extremities because they block receptors involved in other functions like energy regulation and blood vessel dilation. Here, both pharmacokinetics and pharmacodynamics are involved in the experience of side effects.
Types of Side Effects: Predictable, Unpredictable, and Everything In Between
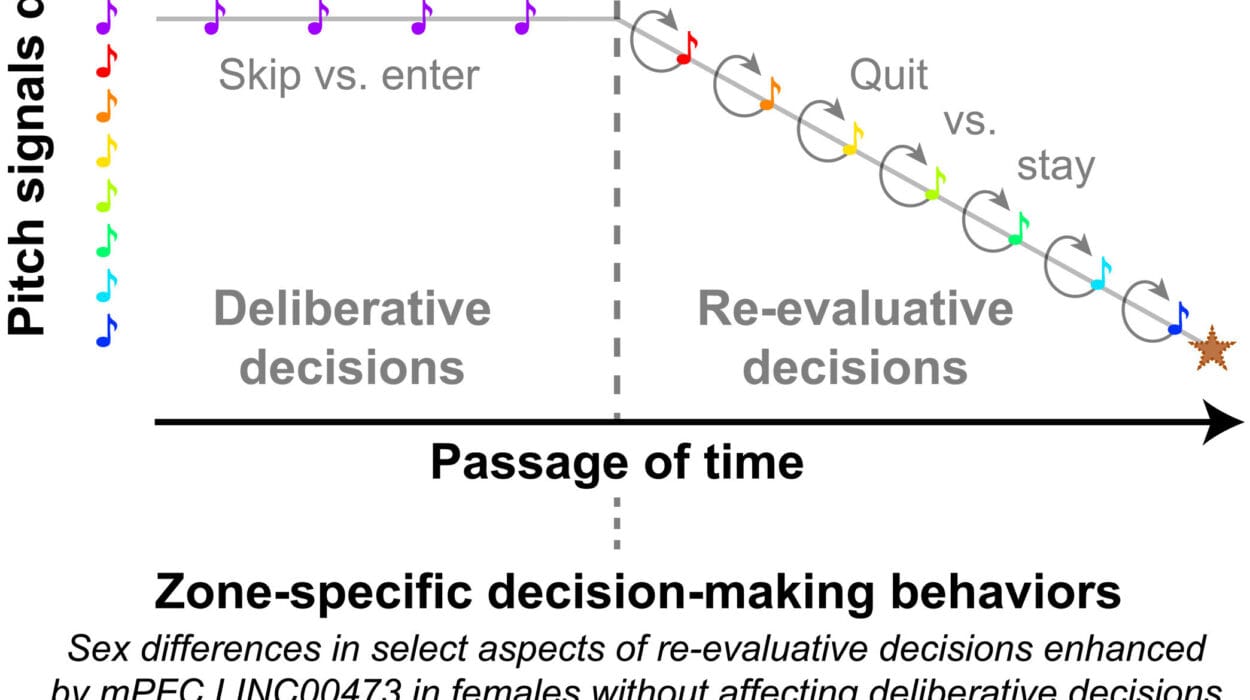
Side effects aren’t a one-size-fits-all phenomenon. They come in many shapes and sizes. Some are expected and well-documented, while others are rare surprises. In clinical medicine, side effects are typically categorized into several types.
One major category is dose-dependent side effects. These occur when too much of a drug is taken or accumulates in the system. The more you take, the more intense the side effect. For instance, a common painkiller like ibuprofen can cause stomach ulcers if used in high doses for a prolonged period.
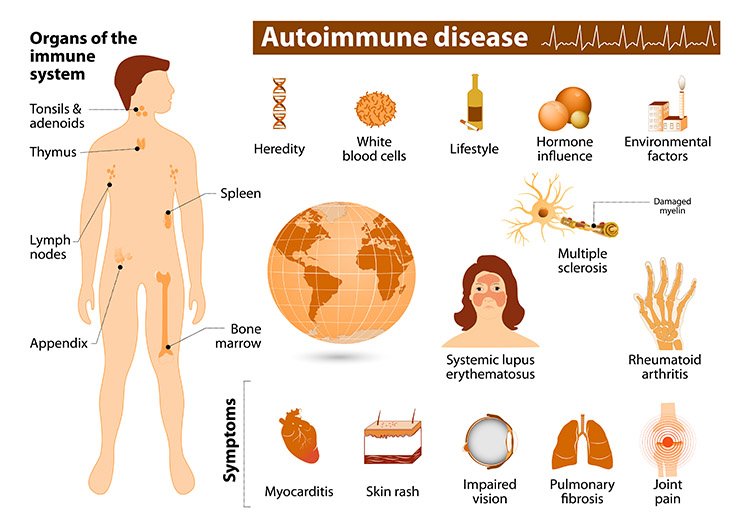
Another type is allergic reactions. These are immune responses to a drug, not because of its intended action, but because the immune system mistakenly sees it as a threat. These can range from mild rashes to severe anaphylaxis, which can be life-threatening.
Idiosyncratic reactions are the wild cards. These are unpredictable, not related to dose, and often tied to an individual’s unique biology or genetic makeup. One person might take a drug with no issues, while another might have a dangerous reaction.
Then there are paradoxical reactions — when a drug causes the opposite effect of what’s expected. A sleeping pill might cause agitation instead of drowsiness in some individuals. These are rare but highlight the complex interactions between brain chemistry and medication.
Genetics and Side Effects: The Rise of Pharmacogenomics
Why do some people experience side effects while others do not? The answer often lies in genetics. Every person metabolizes drugs slightly differently, thanks to variations in genes that encode for liver enzymes, transport proteins, and drug receptors.
This field of study, known as pharmacogenomics, is revolutionizing the way we understand side effects. For example, a variation in the CYP2C9 gene can affect how individuals metabolize warfarin, a common blood thinner. Those with a certain variant may be at higher risk for bleeding complications unless their dosage is adjusted.
Genetic testing is becoming more common in medicine to tailor drug therapy to individual patients. This personalized approach — sometimes called precision medicine — aims to maximize effectiveness while minimizing adverse effects. It’s a future where side effects might be drastically reduced by aligning medications with each patient’s unique genetic profile.
Psychological and Environmental Influences
Side effects aren’t always purely physical. Psychological factors play a surprising role in how we experience medications. The phenomenon known as the “nocebo effect” shows that if a person expects a negative reaction, they are more likely to experience one — even if they are taking a placebo.
Similarly, a person’s mood, stress levels, and environment can influence side effect profiles. Fatigue, for example, might be a symptom of depression, poor sleep, or a medication — and all of these factors can overlap. Disentangling the true cause can be challenging.
The environment also plays a role. Temperature, altitude, hydration, and diet can all alter how a drug is absorbed or processed. Grapefruit juice, for instance, interferes with the metabolism of many medications by inhibiting a key enzyme in the liver. This can lead to unexpectedly high drug levels and increased risk of side effects.
Polypharmacy: When Medications Collide
As people age or develop chronic conditions, they often find themselves taking multiple medications. This practice, known as polypharmacy, increases the risk of drug-drug interactions — one of the leading causes of adverse side effects.
Each drug has its own profile, but when combined, their interactions can amplify effects, reduce effectiveness, or produce entirely new reactions. A sedative and a muscle relaxant might each be safe alone, but together they can depress breathing and cause dangerous drowsiness.
Doctors and pharmacists must be vigilant when prescribing or reviewing medications, especially in elderly patients or those with multiple conditions. Computerized systems and drug interaction checkers are now essential tools in minimizing these risks.
The Importance of Clinical Trials and Post-Marketing Surveillance
Before a drug reaches the public, it undergoes a rigorous series of clinical trials to assess its safety and effectiveness. These trials are conducted in phases, starting with small groups and gradually expanding. Researchers look for side effects and determine acceptable risk levels.
However, no trial can account for every possible outcome. Rare side effects may only emerge after a drug has been used by millions of people. That’s why post-marketing surveillance is critical. Systems like the FDA’s MedWatch or the WHO’s VigiBase allow healthcare professionals and patients to report adverse reactions.
Sometimes, side effects that seem minor in trials become serious in the real world. This has led to several high-profile drug withdrawals. The painkiller rofecoxib (Vioxx), for instance, was removed from the market after it was linked to an increased risk of heart attacks — a side effect that was not fully apparent in early trials.
Managing Side Effects: Strategies for Patients and Providers
The good news is that most side effects are manageable. Open communication between patients and healthcare providers is key. If you experience an unexpected reaction, reporting it promptly can lead to dosage adjustments, alternative medications, or supportive therapies to reduce discomfort.
Sometimes side effects are transient — they appear as the body adjusts to a new medication and fade over time. Others may require long-term strategies. For example, medications that cause nausea might be taken with food, or a drug that causes drowsiness might be scheduled for nighttime use.
Healthcare providers also weigh the risk-benefit ratio. If a medication causes mild side effects but offers life-saving benefits, it may still be the best option. The goal is always to maximize therapeutic gain while minimizing harm.
When Side Effects Become Medical Emergencies
Most side effects are nuisances, but some signal serious problems. Difficulty breathing, swelling of the face or throat, severe rashes, chest pain, or sudden confusion may indicate a medical emergency. These should never be ignored.
Anaphylaxis, liver failure, or severe skin reactions like Stevens-Johnson syndrome are rare but potentially fatal. Patients need to be educated about warning signs and when to seek immediate care. The mantra “better safe than sorry” certainly applies.
Side Effects in the Era of New Therapies
Modern medicine is entering an age of biologics, gene therapy, and personalized drugs. While these innovations hold promise, they also bring new types of side effects. Biologics, which are made from living cells, can trigger immune responses not seen with traditional drugs.
Gene therapy — altering DNA to correct disease — is on the cutting edge, but its long-term effects are still unknown. Even mRNA vaccines, like those developed for COVID-19, presented a new frontier in understanding side effect profiles.
As science evolves, so too must our understanding of how to monitor, report, and mitigate unintended effects. Transparency, vigilance, and patient education remain our best defenses.
Conclusion: Respecting the Double-Edged Sword
Side effects are a reminder that medicine is both art and science — powerful, life-saving, but never without risks. They are the echoes of our biological individuality, the price we sometimes pay for healing, and the clues that lead us to safer, better therapies.
Knowing about side effects doesn’t mean fearing them. It means being informed, cautious, and proactive. It means asking questions, understanding your body, and partnering with healthcare providers for the best possible outcomes.
Every pill, every shot, every treatment carries a story of risk and reward. The challenge of medicine is to tip the scales — to make the benefits outweigh the burdens. And in that balancing act, knowledge is our greatest ally.