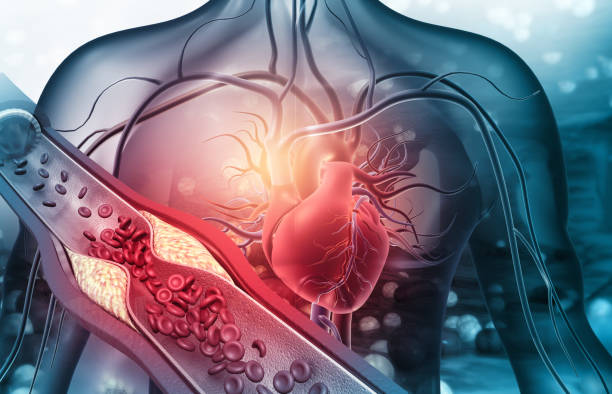
The human body is a marvel of design, and at the heart of it all is an intricate network of blood vessels that serves as a lifeline, delivering oxygen, nutrients, and hormones to every cell. Blood vessels are like highways that transport life-sustaining substances to our organs, tissues, and muscles, and just as a traffic jam can halt the flow of vehicles on a highway, any disruption in the flow of blood can have devastating consequences. This disruption is the essence of vascular disease.
Vascular disease refers to any condition that affects the blood vessels—arteries, veins, and capillaries—that transport blood throughout the body. It’s a broad umbrella term encompassing a wide range of issues, all of which ultimately lead to the same result: a reduction or complete blockage in blood flow. This can occur anywhere in the body, but it most commonly affects the arteries, which carry oxygenated blood away from the heart. When these arteries become narrowed, blocked, or weakened, the consequences can be life-threatening.
In this exploration of vascular disease, we’ll journey through the different types of vascular problems, the factors that contribute to them, and their impact on our health. We’ll also examine the steps that can be taken to prevent, diagnose, and treat these conditions to ensure that the lifeblood of the body flows freely.
The Anatomy of Blood Flow: Arteries, Veins, and Capillaries
Before delving into the specifics of vascular disease, it’s important to understand the components involved in blood circulation. Blood vessels are classified into three main types: arteries, veins, and capillaries.
- Arteries are the thick-walled vessels that carry oxygen-rich blood from the heart to the rest of the body. They are under high pressure because they must carry blood forcefully away from the heart to reach even the most distant tissues.
- Veins carry deoxygenated blood back to the heart. These vessels have thinner walls and are equipped with valves that prevent blood from flowing backward as it travels up from the lower body.
- Capillaries are the smallest blood vessels, serving as the bridge between arteries and veins. They are so thin that red blood cells must pass through them in single file. It is here that the exchange of gases, nutrients, and waste products occurs between the blood and tissues.
The cardiovascular system, as a whole, works like an elaborate pump, ensuring that the tissues and organs receive a steady supply of oxygen and nutrients and are cleared of waste products. But when any part of this system fails to function properly, health problems arise.
The Culprit: Atherosclerosis and Blocked Blood Flow
Atherosclerosis is one of the most common causes of vascular disease and is typically the root cause behind conditions like coronary artery disease (CAD), stroke, and peripheral artery disease (PAD). In essence, atherosclerosis occurs when plaque builds up in the arteries, causing them to narrow and stiffen. This plaque consists of fat, cholesterol, and other substances that accumulate on the inner walls of blood vessels.
Over time, the plaque hardens and thickens, restricting blood flow. This can lead to reduced oxygen supply to vital organs, resulting in chest pain (angina), shortness of breath, or other symptoms of heart disease. If the plaque ruptures, a blood clot may form, potentially leading to a heart attack or stroke.
Atherosclerosis doesn’t develop overnight. It’s a gradual process that can begin in childhood and worsen over decades. In fact, fatty streaks can be seen in the arteries of children as young as 10 years old, and by the time someone reaches their 50s or 60s, atherosclerosis may have progressed to the point where the blood flow is significantly compromised.
The Risk Factors: Who’s at Risk for Vascular Disease?
Vascular disease is not confined to any single group of people. In fact, it affects individuals of all ages, genders, and backgrounds. However, there are certain factors that can significantly increase the risk of developing vascular problems.
1. High Blood Pressure (Hypertension)
Chronic high blood pressure is one of the most significant contributors to vascular disease. When blood pressure is consistently elevated, it can damage the inner walls of the arteries, making them more susceptible to plaque buildup. Over time, this leads to the narrowing and hardening of the arteries. Hypertension also forces the heart to work harder, increasing the risk of heart failure and other cardiovascular issues.
2. Smoking
Smoking is a leading cause of vascular disease. The toxins in cigarette smoke damage the blood vessels, leading to inflammation, narrowing, and clot formation. Smoking also lowers levels of high-density lipoprotein (HDL), the “good” cholesterol, which helps remove fat from the bloodstream. As a result, smoking accelerates the process of atherosclerosis and significantly increases the risk of heart attacks, strokes, and peripheral artery disease.
3. High Cholesterol Levels
Cholesterol is a type of fat found in the blood, and while the body needs it to build cells, too much of it can be harmful. Low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, can contribute to the buildup of plaque in the arteries, leading to atherosclerosis. High levels of LDL cholesterol, combined with low levels of HDL cholesterol, can be a dangerous combination, increasing the risk of cardiovascular disease.
4. Diabetes
Diabetes, particularly when it is poorly managed, can lead to vascular disease by damaging the blood vessels. High blood sugar levels can cause inflammation and narrowing of the arteries, reducing blood flow. This condition, known as diabetic vasculopathy, often leads to peripheral artery disease, heart disease, and kidney damage.
5. Obesity and Physical Inactivity
Obesity is another key factor that contributes to vascular disease. Excess fat, especially abdominal fat, increases the risk of high blood pressure, high cholesterol, and diabetes—each of which is a risk factor for vascular disease. Additionally, a sedentary lifestyle weakens the heart and blood vessels, leading to poor circulation and increased risk of blockages.
6. Family History and Age
Genetics also plays a role in vascular disease. If you have a family history of heart disease, high blood pressure, or stroke, you may be at an increased risk. Age is another significant factor; as we age, our arteries naturally become stiffer, and the likelihood of plaque buildup increases.
7. Gender
Men tend to develop vascular disease earlier in life than women, but after menopause, women’s risk of heart disease and stroke increases significantly. Estrogen, which protects women’s blood vessels during their younger years, decreases after menopause, leaving them more vulnerable to vascular problems.
Symptoms: Recognizing the Warning Signs of Vascular Disease
The symptoms of vascular disease vary depending on which part of the body is affected and how severe the blockage is. Some of the most common symptoms include:
- Chest pain (Angina): When the heart’s blood supply is reduced, it may cause pain or discomfort in the chest. This is commonly associated with coronary artery disease, which is a result of atherosclerosis in the arteries of the heart.
- Shortness of Breath: When the heart or lungs are not receiving enough oxygen, shortness of breath can occur. This is especially common in people with coronary artery disease or heart failure.
- Leg Pain or Cramping: If the blood vessels in the legs become narrowed or blocked, a person may experience pain or cramping, particularly when walking or exercising. This is a hallmark symptom of peripheral artery disease.
- Numbness or Weakness: A blockage in the arteries supplying the brain can cause stroke-like symptoms, including sudden numbness or weakness in the face, arm, or leg, particularly on one side of the body.
- Cold Hands or Feet: If the arteries in the arms or legs become narrowed, circulation can be impaired, causing extremities to feel cold or numb. This can also cause skin color changes.
If you experience any of these symptoms, it’s important to seek medical attention promptly, as they may be signs of vascular disease.
Diagnosis: Uncovering the Hidden Blockages
To diagnose vascular disease, doctors rely on a combination of patient history, physical examination, and diagnostic tests. The first step often involves listening for abnormal sounds, known as bruits, which can indicate turbulent blood flow due to narrowing or blockages. Blood pressure is checked, as well as the pulse in various parts of the body to assess circulation.
Several tests are used to visualize blood flow and identify blockages or areas of concern:
- Ultrasound: This non-invasive test uses sound waves to create images of blood vessels, allowing doctors to detect any narrowing, blockages, or clots.
- Angiography: This procedure involves injecting a contrast dye into the blood vessels and taking X-rays to see the flow of blood. It is particularly useful for detecting blockages in the coronary arteries, brain, or legs.
- CT or MRI Scans: These imaging techniques can also provide detailed images of the blood vessels and help identify areas of blockage or damage.
Treatment: Restoring Healthy Blood Flow
The treatment for vascular disease depends on the type and severity of the condition. In many cases, lifestyle changes such as adopting a healthy diet, exercising regularly, and quitting smoking can significantly improve circulation and reduce the progression of the disease. Medications may also be prescribed to lower blood pressure, reduce cholesterol, or prevent blood clots.
In more severe cases,
surgical intervention may be necessary. Procedures such as angioplasty, where a balloon is used to widen narrowed arteries, or bypass surgery, where a graft is used to bypass blocked arteries, can restore blood flow to critical areas. In some cases, stents may be inserted to keep arteries open.
For individuals with peripheral artery disease, walking programs and medications to manage pain may help. In extreme cases, amputation may be required if blood flow to the limbs is irreparably compromised.
Prevention: Keeping Your Vascular Health in Check
Preventing vascular disease is largely about managing risk factors. Regular exercise, maintaining a healthy weight, eating a balanced diet, controlling blood pressure, and managing cholesterol levels are all crucial steps in preventing vascular problems. For those with diabetes, careful monitoring of blood sugar levels is essential.
Routine check-ups with a healthcare provider can help identify early signs of vascular disease, allowing for prompt treatment and lifestyle adjustments.
Conclusion: Protecting the Lifeblood of the Body
Vascular disease is a complex and often silent condition that can have devastating consequences if left untreated. Whether it affects the heart, brain, or limbs, a reduction or blockage in blood flow can cause irreparable damage to vital organs and tissues. By understanding the causes, symptoms, and treatments for vascular disease, individuals can take proactive steps to protect their vascular health and maintain the free flow of life-giving blood throughout their bodies. With early detection and proper management, the risk of serious complications can be reduced, and the journey toward better health can continue.