Sexually transmitted infections — STIs — are often whispered about, hidden behind closed doors, or buried under layers of stigma. Yet they are among the most common health concerns in the world, affecting people across every continent, culture, and community. They do not discriminate by age, race, gender, or background. They can touch the lives of teenagers exploring their first relationships, couples in long-term partnerships, and older adults who may have thought such risks were long behind them.
The reason STIs matter is not just because they affect millions each year — it’s because of what they represent. They are a mirror reflecting how we, as a society, talk about sex, health, and responsibility. They are also an arena where science, medicine, and public health work tirelessly to protect lives and break chains of transmission.
Understanding STIs is not about fear. It’s about empowerment. It’s about knowing the facts, recognizing symptoms, and taking steps to protect both your health and the health of those you care about. And it’s about dismantling the shame that too often surrounds them, because shame is the enemy of prevention and treatment.
The Landscape of STIs in Today’s World
In the early 21st century, STIs remain one of the most significant public health challenges. The World Health Organization estimates that more than a million new cases occur every single day worldwide. These range from bacterial infections that can be cured with antibiotics to viral infections that can be managed but not eliminated from the body.
What makes STIs particularly complex is that many people who have them show no symptoms at all — yet can still pass them on. This silent spread is why public health experts emphasize regular screening for anyone who is sexually active, not just those who believe they are at risk.
Global mobility, dating apps, and shifting cultural norms have changed how and when people connect. This can increase opportunities for intimacy, but it also means STIs can travel faster and farther than ever before. Yet modern medicine has also given us powerful tools for detection, treatment, and even prevention — from rapid diagnostic tests to preventive vaccines.
What Exactly Is an STI?
An STI is an infection transmitted primarily through sexual contact — including vaginal, anal, and oral sex. Some can also be spread through nonsexual means, such as from mother to baby during childbirth or breastfeeding, or through shared needles.
The term “STI” is often used interchangeably with “STD” (sexually transmitted disease). The distinction is subtle but important: infection refers to the presence of a pathogen in the body, while disease means that infection has caused noticeable symptoms or harm. You can have an STI without showing any signs of illness, which is precisely why they can be so easily passed on without anyone realizing it.
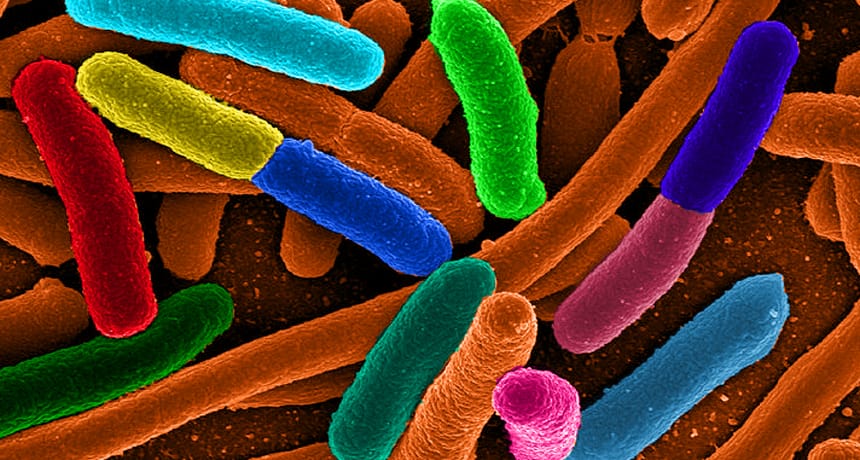
The Science Behind Transmission
To understand how to prevent STIs, it helps to understand how they are transmitted. The pathogens responsible — bacteria, viruses, parasites — are often found in bodily fluids such as blood, semen, vaginal secretions, and saliva. They can also live in mucous membranes or skin in the genital area. During sexual activity, these fluids and tissues can come into contact, allowing the infection to pass from one person to another.
Some infections, like herpes and HPV, can be transmitted even without penetrative sex through skin-to-skin contact. Others, like HIV, require the exchange of specific fluids. The nature of the pathogen determines how easily it spreads and what prevention strategies are most effective.
Common Sexually Transmitted Infections
Some STIs have been recognized for centuries; others have emerged more recently as medical science has improved in identifying them. Among the most common today are chlamydia, gonorrhea, syphilis, trichomoniasis, herpes simplex virus (HSV), human papillomavirus (HPV), and human immunodeficiency virus (HIV).
Bacterial infections such as chlamydia, gonorrhea, and syphilis can often be cured with the right antibiotics if detected early. Viral infections like herpes and HIV cannot be cured, but treatments can control symptoms and dramatically reduce the risk of passing them to others. HPV is a unique case — many strains clear naturally, but others can cause genital warts or lead to cancers.
Knowing which infections are most common in your community can help you make informed decisions about testing and protection, but prevention strategies tend to overlap across most STIs.
Recognizing Symptoms — and Why Silence Is Common
One of the great challenges in STI control is that many infections are “silent.” Chlamydia, for instance, is often called the “silent infection” because most people feel fine despite carrying the bacteria. Gonorrhea and HPV can also lurk without obvious symptoms.
When symptoms do appear, they may include unusual discharge, pain or burning during urination, sores, rashes, itching, swelling, or pain during sex. Some viral infections can cause recurring outbreaks, such as herpes, which manifests as blisters or sores.
However, the absence of symptoms does not mean the absence of infection — nor does it mean the infection is harmless. Untreated STIs can lead to serious health problems, including infertility, chronic pain, increased HIV risk, and certain cancers. This is why regular screening is essential.
The Role of Testing
Testing is the most reliable way to know whether you have an STI. Modern diagnostics range from simple urine tests and swabs to blood tests for viral infections. Some can be done in minutes in a clinic; others may require laboratory analysis.
Many clinics now offer confidential or anonymous testing, and in some countries, home test kits are available. The key is to test regularly if you are sexually active, especially when starting a new relationship or if you have multiple partners. Early detection means early treatment, which protects both you and others.
Treatment and Management
The good news is that many STIs are treatable — and some are entirely curable. Antibiotics can clear bacterial infections like chlamydia, gonorrhea, and syphilis. The challenge comes when infections are left untreated, allowing bacteria to spread and cause long-term damage.
For viral infections like herpes, HIV, and chronic hepatitis B, treatment focuses on managing the infection rather than eliminating it. Antiviral medications can reduce symptoms, control viral load, and prevent transmission. For example, antiretroviral therapy (ART) for HIV can suppress the virus to undetectable levels, meaning it cannot be passed on sexually — a concept known as “U=U” (Undetectable = Untransmittable).
Treatment success depends not only on medication but also on adherence, follow-up, and addressing any co-infections or complications.
Prevention as the First Line of Defense
Preventing STIs is often simpler than treating them. Condoms, when used correctly and consistently, are highly effective in reducing the risk of many infections. Dental dams provide protection during oral sex. Vaccines are available for some viral STIs, including HPV and hepatitis B, offering long-term immunity.
Communication between partners is just as important as physical protection. Discussing STI history, testing, and prevention methods can feel awkward, but it builds trust and helps prevent transmission. Regular screening, even in monogamous relationships, ensures that both partners remain healthy.
Overcoming Stigma and Building a Culture of Openness
Perhaps the greatest barrier to tackling STIs is not the infections themselves, but the stigma attached to them. Shame can prevent people from seeking testing, telling partners, or even acknowledging their risk. This stigma is rooted in misconceptions about morality, sexual behavior, and personal worth.
Changing this requires cultural shifts — in how we educate young people about sexual health, in how healthcare providers talk to patients, and in how we as individuals react to STI diagnoses. These infections are medical conditions, not moral judgments. Addressing them openly allows for early treatment, honest conversations, and healthier communities.
The Future of STI Prevention and Treatment
Medical science continues to advance in the fight against STIs. Researchers are developing new vaccines, including ones for herpes and HIV. Rapid testing technologies are making it easier to diagnose infections on the spot. Long-acting injectable medications may soon provide months of protection or treatment with a single dose.
Public health strategies are also evolving, with more emphasis on integrating STI services into general healthcare, reaching underserved populations, and using digital tools to connect people with testing and treatment. These innovations, combined with education and awareness, offer hope for reducing the global burden of STIs.
Living Well After Diagnosis
An STI diagnosis is not the end of a healthy sexual or romantic life. With the right treatment and self-care, most people go on to have fulfilling relationships. Managing an STI often involves taking medication, making informed choices about intimacy, and staying engaged with healthcare providers.
Support networks, whether friends, partners, or support groups, can make a significant difference in emotional well-being. Education empowers people to navigate relationships confidently, knowing that they can protect themselves and others.
A Final Word — Knowledge Is Power
Understanding STIs is not about instilling fear; it’s about replacing fear with facts. It’s about turning silence into dialogue, and stigma into support. The more we know, the better we can protect ourselves and each other.
Sex is a part of human life — so is sexual health. Recognizing that STIs are preventable, treatable, and manageable is the first step toward a healthier, more informed future. The next step is ours to take: get informed, get tested, and talk openly.