Every human carries a story written not on paper but deep within the cells of their body. This story is told in DNA—a long, winding molecule that encodes the instructions for life itself. From the color of your eyes to the way your body metabolizes sugar, DNA quietly shapes who you are. But alongside the traits we cherish, this genetic script can also carry vulnerabilities—tiny changes in the code that may lead to disease.
Inherited conditions have fascinated and frightened humanity for centuries. In medieval villages, families who passed down a mysterious ailment were whispered about in hushed tones. In royal courts, dynasties struggled with bleeding disorders that changed the course of empires. Even today, despite modern medicine, people live with genetic diseases that they have inherited from parents and ancestors long gone.
Understanding the genetics of disease is not merely an academic pursuit; it is deeply personal. It is the science of why certain illnesses appear generation after generation. It is the hope of parents wanting to know whether their child will be healthy. It is the story of humanity grappling with its own biological heritage and seeking ways to heal without altering what makes us unique.
The Blueprint of Life: DNA and Genes
To understand inherited disease, we must first understand the machinery of life. At the heart of every human cell lies the nucleus, and within it, the chromosomes—long, thread-like structures made of DNA. Each human cell carries 23 pairs of chromosomes, one set from each parent, for a total of 46.
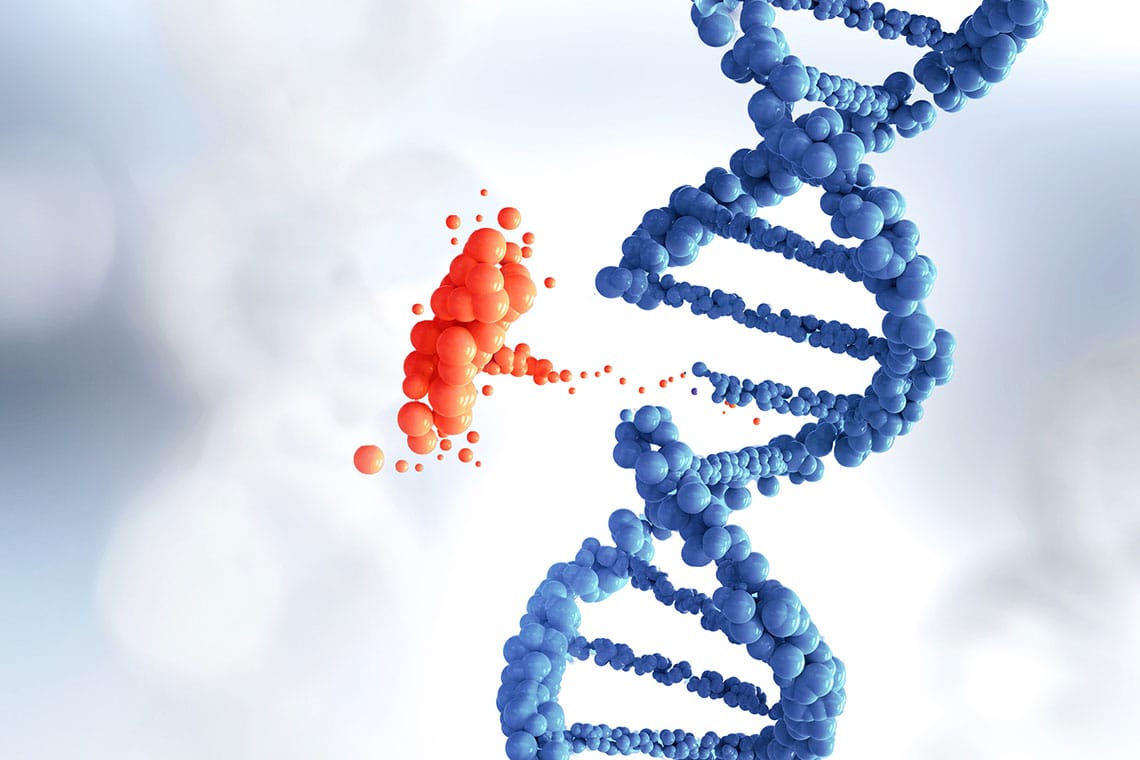
DNA itself is a twisted ladder, a double helix formed by chemical bases—adenine, thymine, cytosine, and guanine. Arranged in a precise sequence, these bases form genes, which act as instructions for building proteins. Proteins, in turn, are the molecular workers of the body, forming structures, transmitting signals, and carrying out the countless processes that keep us alive.
Remarkably, humans have about 20,000 genes, yet subtle differences in these genes—called variants or mutations—can profoundly influence health. Some variants have no effect, others are beneficial, but some disrupt normal function, leading to disease.
Inheritance: The Flow of Genetic Information
When a child is conceived, they inherit half of their chromosomes from the mother and half from the father. This blending of genetic material is why children resemble their parents yet remain unique individuals. However, it also means that genetic variants—whether harmless or harmful—can be passed from one generation to the next.
Inherited diseases follow certain patterns of inheritance. Mendelian inheritance, named after the monk Gregor Mendel who discovered the principles of genetics, describes how traits and conditions can be dominant or recessive. In dominant conditions, a single altered copy of a gene is enough to cause disease, while in recessive conditions, both copies must be altered. There are also conditions linked to sex chromosomes, known as X-linked or Y-linked disorders.
Beyond these simple patterns lies a complex web of polygenic diseases, where multiple genes contribute to risk, often interacting with environmental factors. This complexity makes understanding inherited diseases both challenging and fascinating.
The Many Faces of Genetic Disease
Genetic diseases are as varied as the human genome itself. Some appear at birth, others emerge later in life. Some affect only a single organ, while others ripple through entire bodily systems.
Monogenic diseases result from mutations in a single gene. Cystic fibrosis, for example, is caused by alterations in the CFTR gene, leading to thick mucus buildup in the lungs and digestive tract. Sickle cell anemia arises from a single change in the hemoglobin gene, distorting red blood cells into sickle shapes that cause pain and organ damage. Huntington’s disease is a devastating neurodegenerative disorder caused by an expansion of a DNA repeat in a single gene.
Polygenic diseases, on the other hand, involve many genes and are influenced by lifestyle and environment. Diabetes, heart disease, and many cancers fall into this category. The inheritance of these conditions is more subtle; a person may inherit a predisposition but never develop the disease unless other factors intervene.
Some genetic disorders are chromosomal, arising from structural changes in chromosomes themselves. Down syndrome occurs when there is an extra copy of chromosome 21. Turner syndrome and Klinefelter syndrome involve missing or additional sex chromosomes.
How Mutations Arise
Mutations are changes in the DNA sequence. Some are inherited from parents, while others occur spontaneously during life. They can result from errors in DNA replication or from external influences like radiation, chemicals, or viruses.
Not all mutations are harmful. Many have no effect at all, and some even provide advantages, such as resistance to certain infections. But when a mutation alters a critical gene, it can disrupt the protein it encodes, leading to malfunction and disease.
Certain regions of DNA are more prone to mutations, known as hotspots. Some genes are particularly vulnerable because they are large or involved in processes where even a small change can have dramatic effects.
Epigenetics: Beyond the DNA Sequence
While genetic mutations change the DNA code, another layer of regulation exists: epigenetics. Epigenetic changes do not alter the DNA sequence itself but affect how genes are expressed—whether they are turned on or off.
Chemical tags called methyl groups can attach to DNA, silencing genes, while modifications to histone proteins can open or close access to the genetic code. These changes can be influenced by diet, stress, toxins, and other environmental factors. In some cases, epigenetic alterations can be passed to future generations, adding another dimension to inherited disease.
Epigenetics helps explain why identical twins, with the same DNA, can show differences in health and disease. It also opens doors to potential therapies that target gene expression without altering the underlying genetic sequence.
The Human Impact of Inherited Conditions
Behind every genetic disease is a human story. A parent watching their child struggle with muscular dystrophy. A teenager learning they carry a gene for a disorder that may strike in adulthood. A couple making difficult choices after genetic testing reveals risks for future children.
These conditions do more than affect health—they shape identity, relationships, and family histories. Genetic diseases can bring fear and uncertainty, but also resilience and community, as families support one another and advocate for research and treatment.
The emotional weight of inherited disease is heavy, yet knowledge can empower. Genetic counseling helps individuals understand risks, options, and support networks. Advances in diagnostics and therapies offer hope where once there was little.
Unlocking the Genome: Tools of Modern Genetics
The last century has transformed our understanding of genetics. From Mendel’s pea plants to the discovery of DNA’s structure, each discovery opened new windows into inheritance. But nothing compared to the Human Genome Project—a monumental effort completed in 2003 that mapped the entire human genetic code.
This achievement ushered in an era of genomic medicine. Today, whole-genome sequencing allows doctors to identify mutations causing rare diseases in children. Targeted genetic tests can reveal carrier status for conditions like Tay-Sachs or sickle cell disease. Prenatal testing can detect chromosomal abnormalities before birth.
Powerful laboratory tools like CRISPR now allow scientists to edit genes directly, offering the potential to correct mutations. Though gene editing in humans remains ethically and technically complex, it holds promise for treating conditions once deemed incurable.
Genetic Testing: Knowledge and Choice
Genetic testing has become increasingly accessible. With a simple blood or saliva sample, individuals can learn about inherited risks, carrier status, or the likelihood of passing on certain conditions.
For families with a history of genetic disease, this information can be life-changing. It enables informed decisions about family planning, early interventions, or participation in clinical trials. But it also raises ethical and emotional challenges: How much should we know? Could knowledge of future disease change how we live today?
Privacy and discrimination are real concerns. Genetic information must be handled carefully to protect individuals from misuse, such as employment or insurance bias. As testing becomes more common, society must balance the benefits of knowledge with respect for autonomy and confidentiality.
Therapies and Hope: Treating Genetic Diseases
For many years, inherited diseases were seen as fate—unchangeable consequences of the DNA we inherit. But recent advances are rewriting that narrative.
Gene therapy introduces correct copies of defective genes, offering cures for diseases like spinal muscular atrophy and certain forms of blindness. Researchers are developing therapies for sickle cell anemia and hemophilia that could transform lives.
RNA-based treatments, such as antisense oligonucleotides, can modify how genes are read, bypassing mutations or silencing harmful genes. CRISPR gene editing has already been used experimentally to repair defective DNA in living patients, a groundbreaking step toward permanent cures.
Not all therapies involve direct genetic changes. Many treatments focus on managing symptoms or preventing complications. Early detection, physical therapy, specialized diets, and medications tailored to genetic profiles can greatly improve quality of life.
The Interplay of Genes and Environment
Inherited conditions do not exist in isolation. Even for diseases with strong genetic causes, environment and lifestyle can influence outcomes. Someone with a genetic predisposition to type 2 diabetes may never develop it with careful diet and exercise. Conversely, environmental toxins can trigger illness in genetically susceptible individuals.
This interplay highlights the complexity of health. Genes set the stage, but environment writes much of the play. Understanding both is essential for preventing and treating disease.
Looking Ahead: The Future of Genomic Medicine
The frontier of genetics is vast and rapidly advancing. As sequencing becomes cheaper and more precise, personalized medicine will allow treatments tailored to each individual’s genetic makeup. Doctors will not only treat disease but predict and prevent it long before symptoms appear.
Stem cell research combined with genetic engineering may one day replace defective tissues and organs. Advances in computational biology and artificial intelligence will uncover hidden patterns in genetic data, linking genes to diseases in ways humans alone could not see.
Ethical questions will grow in importance. Should we edit embryos to remove disease-causing genes? How do we ensure equitable access to genetic therapies? What does it mean to change human heredity? Society must navigate these questions carefully to use genetic knowledge responsibly.
Living With Our Genetic Heritage
Ultimately, understanding inherited conditions brings us face to face with what it means to be human. We are products of ancient genetic lineages, carrying both gifts and burdens passed down through time. Our DNA is not destiny, but it shapes the possibilities of our lives.
Families facing genetic disease embody extraordinary courage. They teach us resilience, the power of love and community, and the drive to seek cures not only for themselves but for generations yet to come.
Science offers hope that we may one day heal inherited diseases, but it also reminds us of our shared humanity. In every cell, in every thread of DNA, we are linked—not only to our parents and children but to all life on Earth. The genetics of disease is a story not of flaws but of connection, adaptation, and the ongoing quest to understand and improve the human condition.