Each year, nearly two million people in the United States receive a life-saving implant—small, mesh-like tubes called stents that prop open narrowed or blocked arteries. For many, these silent sentinels in the bloodstream mark a turning point: from breathlessness to breath, from risk to reassurance. But what happens next? Once implanted, these devices remain hidden beneath layers of skin and tissue, their condition largely out of sight—unless a problem arises.
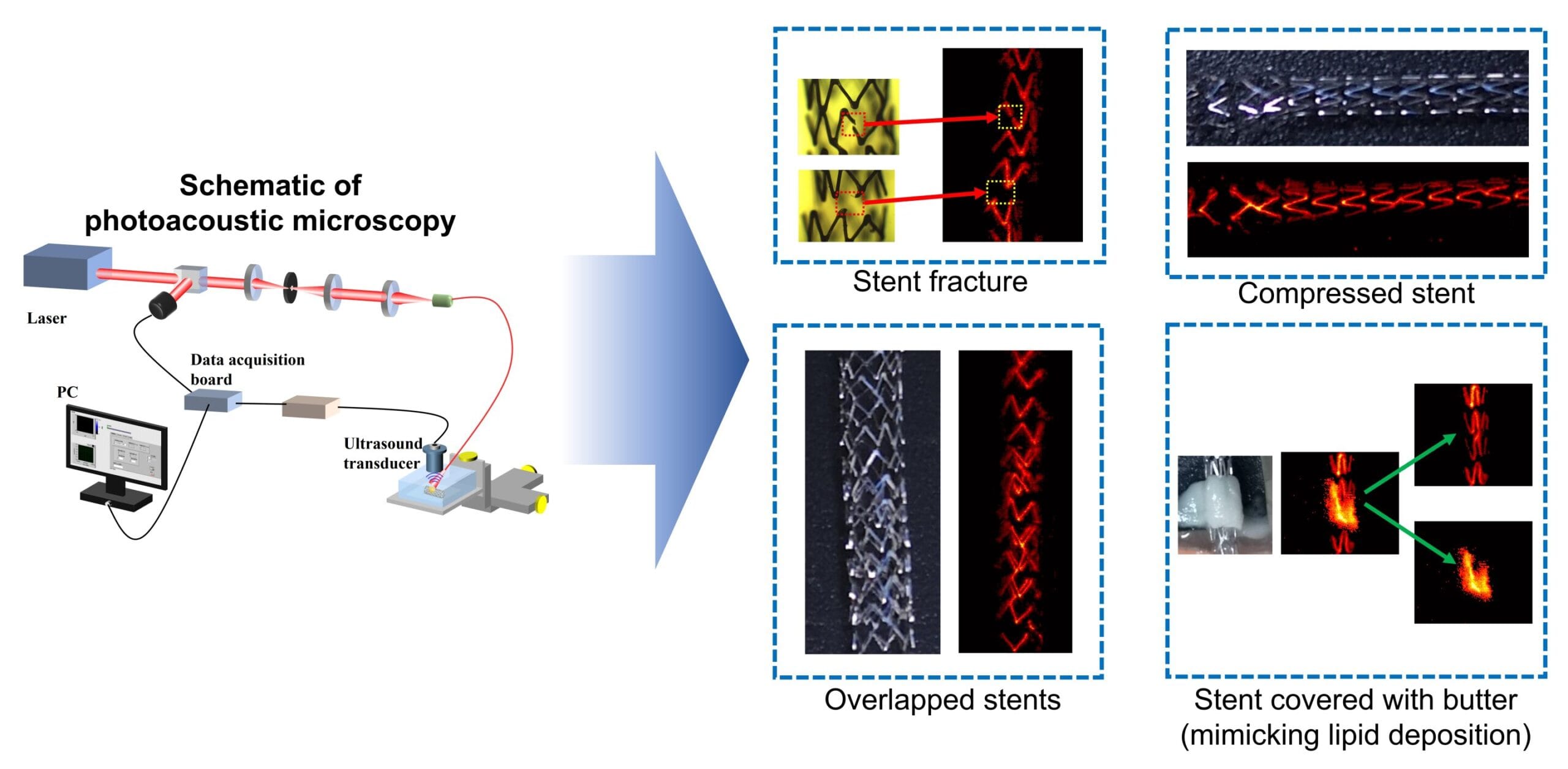
Monitoring stents has always been a challenge. Conventional methods like angiography or CT scans involve radiation, contrast dyes, or invasive procedures. But now, a pioneering breakthrough may bring new light—and sound—to this invisible world. In a study published in Optics Letters, researchers have demonstrated that photoacoustic microscopy (PAM) can, for the first time, image stents noninvasively through the skin. It’s an innovation that could dramatically change how doctors monitor these devices, offering safer, more accessible care for millions.
An Invisible Problem
Despite their ubiquity and critical function, stents are far from risk-free. Over time, they can fracture, become compressed, or shift out of place. They can even trigger the buildup of plaque or blood clots, leading to new blockages. Detecting these complications early can be the difference between timely intervention and life-threatening events like heart attacks or strokes.
Traditionally, imaging these internal structures has required invasive procedures or exposure to X-rays. Tools such as fluoroscopy or intravascular ultrasound, while effective, are resource-intensive and not ideal for frequent or routine monitoring. This creates a clinical dilemma: how do you keep watch over something so vital when seeing it is so difficult?
This was the question that inspired Myeongsu Seong of Xi’an Jiaotong-Liverpool University and Sung-Liang Chen of Shanghai Jiao Tong University to explore an entirely different kind of solution—one that listens rather than probes, one that hears the invisible.
Seeing with Sound: The Power of Photoacoustics
Photoacoustic imaging is a hybrid technology that bridges the realms of light and sound. It begins with light—specifically, short pulses of laser light—fired into biological tissue. When certain molecules absorb this light, they heat up slightly and expand, generating ultrasonic waves. These waves then travel back through the tissue and are captured by an ultrasound transducer. The result is a high-resolution image constructed from how sound is emitted after light is absorbed.
Unlike traditional optical imaging, which is limited by how far light can travel without scattering, photoacoustic imaging takes advantage of sound’s superior ability to penetrate tissue, making it possible to visualize structures buried deeper beneath the skin. And unlike X-ray or MRI, it doesn’t require contrast dyes, ionizing radiation, or bulky, expensive equipment.
“In theory, photoacoustic microscopy could allow us to peer into the body in a noninvasive way—and now, we’ve shown it can be used to view stents,” said Seong. For a technology often used in preclinical imaging of blood vessels or tumors, this new application marks a major milestone.
A Mouse-Sized Experiment with Human-Sized Implications
To test their hypothesis, the researchers created a series of experimental scenarios using stents placed beneath excised mouse skin, simulating what they might look like beneath human skin. These stents were subjected to various conditions: fractures, overlapping segments, and even simulated clots or lipid plaques made from butter. While this might sound unorthodox, the fat in butter mimics the optical properties of human plaque—an inventive and surprisingly effective stand-in.
The imaging was performed at two specific wavelengths: 670 nanometers and 1210 nanometers, each selected for how different materials absorb light. Metal, fat, and tissue all respond differently at various wavelengths, which helps distinguish between them. This is known as spectroscopic photoacoustic imaging—using multiple wavelengths to decode tissue composition.
“The most exciting part was that we could clearly differentiate between the stent and the mock plaque,” Seong explained. “It means we’re not just seeing shapes—we’re seeing what those shapes are made of.” That’s critical in a clinical setting, where distinguishing a dangerous clot from normal tissue can dictate urgent treatment decisions.
From the Surface to the Depths
While photoacoustic microscopy works well for imaging shallow structures—those within a few millimeters of the skin’s surface—what about deeper-placed stents, like those in the carotid arteries or coronary vessels? For that, the researchers point to photoacoustic computed tomography (PACT), a related technique capable of deeper tissue imaging. While PAM provides high resolution in superficial layers, PACT sacrifices some resolution in exchange for greater imaging depth, making it more suitable for larger or more deeply buried arteries.
But even with these technical limitations, PAM could already serve a vital role. For instance, dialysis access sites, often located just under the skin in the arms of patients with kidney failure, frequently require stenting. These superficial stents could be ideal targets for PAM-based monitoring—potentially performed during regular outpatient visits.
Towards a Safer Future in Cardiovascular Care
Though the current results are based on ex vivo experiments (i.e., outside of a living body), the path to clinical application is clear. The next steps involve in vivo animal studies, followed by carefully designed clinical trials in humans. These studies would validate the safety and accuracy of PAM in real-world scenarios, accounting for challenges such as tissue movement, blood flow, and varying skin thickness.
Furthermore, optimizing the imaging system for different body regions will be essential. Stents in legs, arms, or even the heart present different acoustic and optical environments. Tailoring the photoacoustic system—its laser wavelengths, pulse duration, detector sensitivity, and image processing algorithms—will be key to achieving reliable, clinically useful results.
The researchers remain optimistic. “With further refinement, we believe this technique could become part of a doctor’s toolkit—offering a way to see inside the body without cutting it open or exposing it to radiation,” said Chen.
Science That Hears What the Eye Can’t See
Perhaps what makes this breakthrough most remarkable is the way it redefines how we think about imaging. For centuries, medicine has relied on the visible: the incision, the microscope, the X-ray. Now, with photoacoustic technology, we’re entering a new era—one in which we listen to the internal echoes of light and use sound as a guide through the darkness.
It’s a subtle, almost poetic shift. Instead of invading the body to check on a stent, we might one day simply scan the surface, letting light and sound do the rest. No pain. No radiation. Just knowledge—quiet, clear, and profoundly powerful.
The stents we place inside the body are small marvels of engineering, silent guardians of life. But their silence need not mean invisibility. Thanks to the tireless work of these researchers, we are one step closer to a future where every heartbeat, every artery, every hidden threat can be seen, heard, and understood—without a single incision.
Reference: Siqi Liang et al, Photoacoustic microscopy for visualization of stents in multiple scenarios, Optics Letters (2025). DOI: 10.1364/OL.564778