The human body is a universe of hidden relationships, where nutrients, hormones, and microscopic organisms interact in ways that scientists are only beginning to understand. A recent clinical trial from Vanderbilt University Medical Center has revealed one such relationship that could reshape our approach to preventing one of the most common and deadly cancers worldwide: colorectal cancer.
At the heart of this discovery lies magnesium, a mineral most of us associate with bone strength, heart health, or energy production. But magnesium, it turns out, may also play a vital role in shaping our gut microbiome—the vast ecosystem of bacteria that inhabit the digestive tract—and in doing so, influence the body’s defenses against cancer.
Magnesium’s Unexpected Role in Vitamin D Metabolism
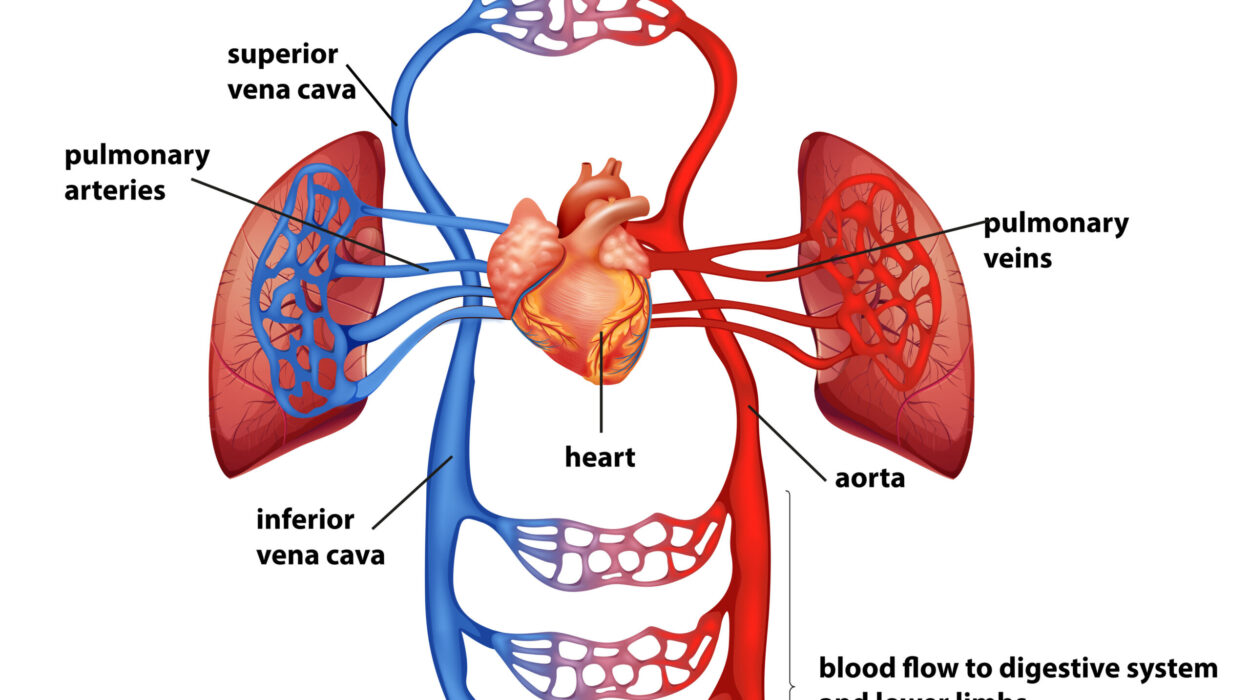
Vitamin D has long been recognized as essential for bone health, immune function, and possibly even cancer prevention. Most of us think of it as “the sunshine vitamin,” produced in our skin when exposed to sunlight and further supported by diet or supplementation. But new evidence shows that vitamin D can also be synthesized locally in the gut, not just in the bloodstream, and that magnesium is a critical partner in this process.
Researchers previously found that magnesium supplements can enhance vitamin D synthesis in the blood, especially when vitamin D levels are low. The new trial reveals something even more intriguing: magnesium also boosts certain gut bacteria that themselves are capable of synthesizing vitamin D. This means that magnesium may support a unique, localized form of vitamin D production inside the digestive tract—one that never makes it into circulation but instead acts directly at the site where colorectal cancer originates.
A Precision-Based Clinical Trial
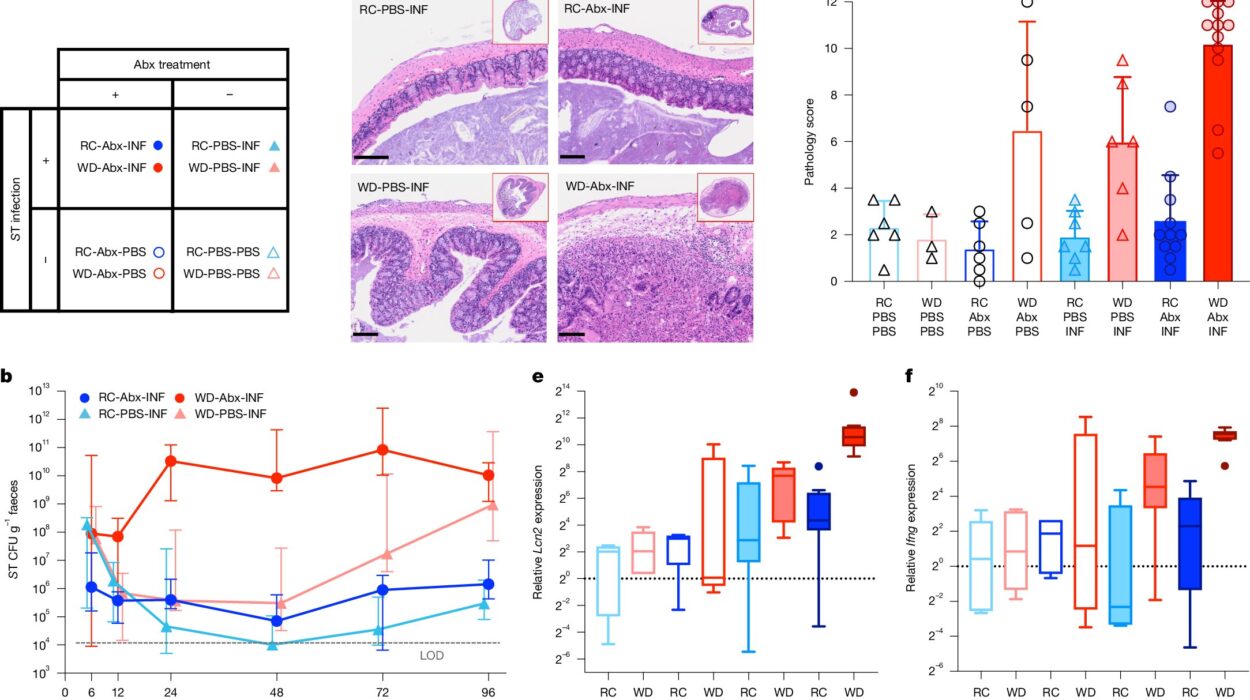
The study, published in The American Journal of Clinical Nutrition, was part of the Personalized Prevention of Colorectal Cancer Trial. It involved 236 participants, all of whom had a history of colorectal polyps—an established risk factor for colorectal cancer. Participants were randomly assigned to receive either a magnesium supplement or a placebo. Over the course of the study, their gut microbiomes were closely monitored using stool samples, rectal swabs, and rectal tissue biopsies. Colonoscopies were also performed after a median follow-up period of 3.5 years.
The results were striking. In individuals with adequate function of a gene called TRPM7, magnesium supplementation increased the abundance of two beneficial gut bacteria: Carnobacterium maltaromaticum and Faecalibacterium prausnitzii. These microbes have previously been shown to work together to boost vitamin D levels and suppress the cellular changes that can lead to colorectal cancer.
The Gender Difference: The Role of Estrogen
Interestingly, the effect of magnesium supplementation was most pronounced in female participants. The researchers believe estrogen may explain this difference. Estrogen appears to shift magnesium from the bloodstream into cells, thereby enhancing magnesium’s local impact on the gut microbiome. This finding highlights a broader truth: the effectiveness of nutritional interventions often depends on individual factors such as sex, genetics, and hormone levels. What works for one group may not work the same way for another.
The Gene-Mineral Connection
The TRPM7 gene emerged as a key player in this study. TRPM7 is essential for regulating the uptake of magnesium and calcium—two minerals critical for cellular health. Participants with adequate TRPM7 function benefited most from magnesium supplementation, showing increased populations of protective gut bacteria. But among participants with inadequate TRPM7 function, the story was more complicated. In these individuals, magnesium actually reduced levels of Faecalibacterium prausnitzii in rectal tissue, raising the possibility that not everyone responds the same way to supplementation.
This highlights the importance of precision medicine: tailoring treatments based on genetic and biological differences rather than assuming a one-size-fits-all solution. In the future, a person’s TRPM7 genotype could help doctors decide whether magnesium supplementation will reduce, or possibly even increase, their cancer risk.
Polyps, Microbes, and Cancer Risk
Among the participants who underwent colonoscopy after the trial, the data revealed a critical link between gut microbes and polyp recurrence. Higher levels of Faecalibacterium prausnitzii in rectal tissue were associated with nearly a threefold increase in the development of additional polyps. At first glance, this seems counterintuitive—why would a bacterium considered beneficial be linked to more polyps? The researchers suggest that context matters. In the presence of adequate TRPM7 function and balanced microbial interactions, F. prausnitzii may be protective. But when this balance is disrupted, the same bacterium could behave differently, underscoring the complexity of the gut ecosystem.
A New Pathway for Cancer Prevention
What makes this research particularly exciting is the possibility of targeting colorectal cancer prevention not just through surgery, chemotherapy, or traditional supplements, but through the modulation of the gut microbiome with something as simple as magnesium. Unlike aggressive treatments, dietary interventions are relatively low-cost, widely available, and generally safe. If future studies confirm these findings, magnesium supplementation could become part of a personalized strategy for individuals at high risk of colorectal cancer.
Nutrition Meets Genetics Meets Microbiology
This trial embodies the future of medicine: an integrated approach that recognizes the interplay between diet, genes, hormones, and the microbiome. Colorectal cancer, once thought of as a disease driven primarily by genetics and environmental exposures, is increasingly understood as a condition influenced by the complex ecology of the gut. Nutrients like magnesium are not acting in isolation; they are part of a vast network of interactions that shape health and disease.
The implications extend beyond colorectal cancer. If magnesium can influence vitamin D synthesis and gut microbiota, what other nutrients may have similar hidden roles? Could calcium, zinc, or iron also influence microbial populations in ways that affect disease risk? These are the kinds of questions researchers are beginning to explore.
The Human Impact
Scientific details aside, what matters most is the human story. Colorectal cancer is the second leading cause of cancer-related deaths worldwide. Behind every statistic are families, communities, and individuals facing the fear and pain of diagnosis and treatment. Preventing even a fraction of these cases would mean fewer hospitalizations, fewer surgeries, fewer lives cut short.
Magnesium, a simple mineral often overlooked in daily nutrition, may offer a key to prevention. And perhaps more importantly, this research offers hope—a reminder that breakthroughs in health do not always come from high-tech machines or futuristic drugs. Sometimes they come from re-examining the everyday elements of life: the food we eat, the minerals in our diet, the invisible ecosystems inside us.
Looking Ahead
While this trial is groundbreaking, it is also just the beginning. Larger studies are needed to confirm the results and to better understand the nuances of magnesium’s effects across different populations. Researchers must also explore the long-term safety of supplementation in those with different TRPM7 genotypes. But the foundation has been laid.
The story of magnesium and colorectal cancer prevention is a powerful example of how modern science is evolving. It shows us that medicine is no longer just about treating disease once it appears—it is about predicting, preventing, and personalizing health strategies before illness takes hold.
Conclusion: A Precision-Based Future
The Vanderbilt study is more than just another piece of medical research—it is a glimpse into a future where prevention is tailored, precise, and profoundly human. By revealing how magnesium shapes gut bacteria, vitamin D synthesis, and cancer risk, it connects the dots between nutrition, genetics, and microbiology in ways that could save lives.
What is most inspiring is the sense of possibility it creates. If something as humble as magnesium can tip the balance in the fight against colorectal cancer, then the door is wide open for other discoveries waiting in plain sight. Science, after all, is about seeing connections where none were seen before—and using that knowledge to create a healthier, more hopeful future.
More information: Elizabeth Sun et al, Magnesium Treatment Increases Gut Microbiome Synthesizing Vitamin D and Inhibiting Colorectal Cancer: Results from a Double-Blind Precision-based Randomized Placebo-Controlled Trial, The American Journal of Clinical Nutrition (2025). DOI: 10.1016/j.ajcnut.2025.09.011