When the world first faced the outbreak of COVID-19, most of the attention was on survival: the immediate threat of a virus that could overwhelm lungs, strain hearts, and claim lives with startling speed. But as the pandemic evolved, another story began to emerge—one of persistence. Many who had recovered from the initial infection found themselves haunted by lingering symptoms that refused to fade, weeks or even months later. This condition has become known as “Long COVID,” or post-acute sequelae of SARS-CoV-2 infection (PASC).
Long COVID is not rare. Studies suggest that millions worldwide have experienced it, and women, in particular, appear to be disproportionately affected. Unlike the sharp crisis of the acute illness, Long COVID is subtle, unpredictable, and often invisible. It can alter daily life, disrupt careers, strain relationships, and test resilience in ways that outsiders may not immediately recognize. For women, whose biological, social, and caregiving roles intersect uniquely, the burden can be especially heavy.
This article explores the intersection of Long COVID and women’s health—its symptoms, its toll, paths to recovery, and the moments when seeking medical care becomes not only advisable but essential.
Why Women Are More Vulnerable
Science is still unraveling the reasons why women seem more likely than men to experience Long COVID. Emerging evidence suggests several possible explanations, though no single factor tells the full story.
One theory involves the immune system. Women generally mount stronger immune responses than men, a trait that helps protect them from some infections but can also predispose them to autoimmune reactions—where the immune system mistakenly attacks the body’s own tissues. Long COVID may, in part, resemble such autoimmune activity, with inflammation persisting long after the virus is gone.
Hormonal differences may also play a role. Estrogen influences immune regulation, cardiovascular health, and even the nervous system. Fluctuations in hormones—during menstrual cycles, pregnancy, or menopause—could shape how the body responds to infection and recovery.
Beyond biology, gendered social roles amplify the impact. Women are often caregivers for children, partners, or aging relatives. They are overrepresented in frontline jobs like healthcare, teaching, and service industries, where exposure to COVID-19 was higher. When symptoms linger, women may also face skepticism from healthcare providers who dismiss complaints as stress or anxiety, compounding the challenge of seeking effective treatment.
Symptoms That Refuse to Fade
Long COVID is not a single illness but a constellation of symptoms that vary from person to person. For women, these symptoms often cluster in ways that make daily life exhausting.
Fatigue is perhaps the most common, described not as ordinary tiredness but as a crushing, bone-deep exhaustion that does not improve with rest. It can make even simple tasks—cooking dinner, walking upstairs, focusing on a work assignment—feel impossible.
Cognitive impairment, often called “brain fog,” is another hallmark. Women report difficulty with memory, concentration, and processing speed. It can feel like words slip just out of reach, like thoughts scatter before they solidify. This symptom is especially disruptive for working women and mothers who juggle multiple responsibilities.
Cardiovascular symptoms, including palpitations, dizziness, and postural orthostatic tachycardia syndrome (POTS), are more frequently reported by women. Standing up may trigger a racing heartbeat, lightheadedness, or near-fainting episodes, making ordinary movement a source of anxiety.
Respiratory symptoms, such as shortness of breath and chest tightness, persist for some, even without visible damage on scans. Women who once exercised easily may find themselves gasping after short walks.
Other symptoms include joint pain, headaches, menstrual irregularities, loss of taste or smell, gastrointestinal issues, and disrupted sleep. The range is so wide that Long COVID sometimes feels like a shifting puzzle, with new pieces appearing as others fade.
The Emotional and Mental Toll
Beyond the physical symptoms, Long COVID weighs heavily on mental and emotional well-being. For women, this burden can be amplified by societal expectations.
An active mother may suddenly struggle to keep up with her children, leading to guilt and frustration. A professional may find her career stalling as concentration wanes. Relationships may strain under the weight of an invisible illness that others cannot see or fully understand.
Depression and anxiety are common, not only as natural reactions to chronic illness but also potentially as direct neurological consequences of the virus itself. For women, whose emotional labor often goes unacknowledged, the added stress of Long COVID can create an overwhelming sense of isolation.
Long COVID Across Life Stages
The impact of Long COVID on women is not uniform—it shifts depending on life stage.
In younger women, symptoms may disrupt education, early careers, or plans for pregnancy. Concerns about fertility or the safety of conceiving while dealing with lingering illness add another layer of anxiety.
For women in midlife, especially those balancing work and caregiving, Long COVID can derail stability. The overlap with perimenopausal symptoms—fatigue, brain fog, irregular periods—can make it difficult to distinguish cause and effect, complicating diagnosis and care.
In older women, Long COVID compounds the risks of aging. It can accelerate frailty, worsen existing conditions like heart disease or diabetes, and diminish independence.
The Path Toward Recovery
Recovery from Long COVID is rarely linear. Some women experience gradual improvement, others fluctuate with “good days” and “crash days,” and still others remain stuck in persistent symptoms for months. Yet recovery, though slow, is possible for many.
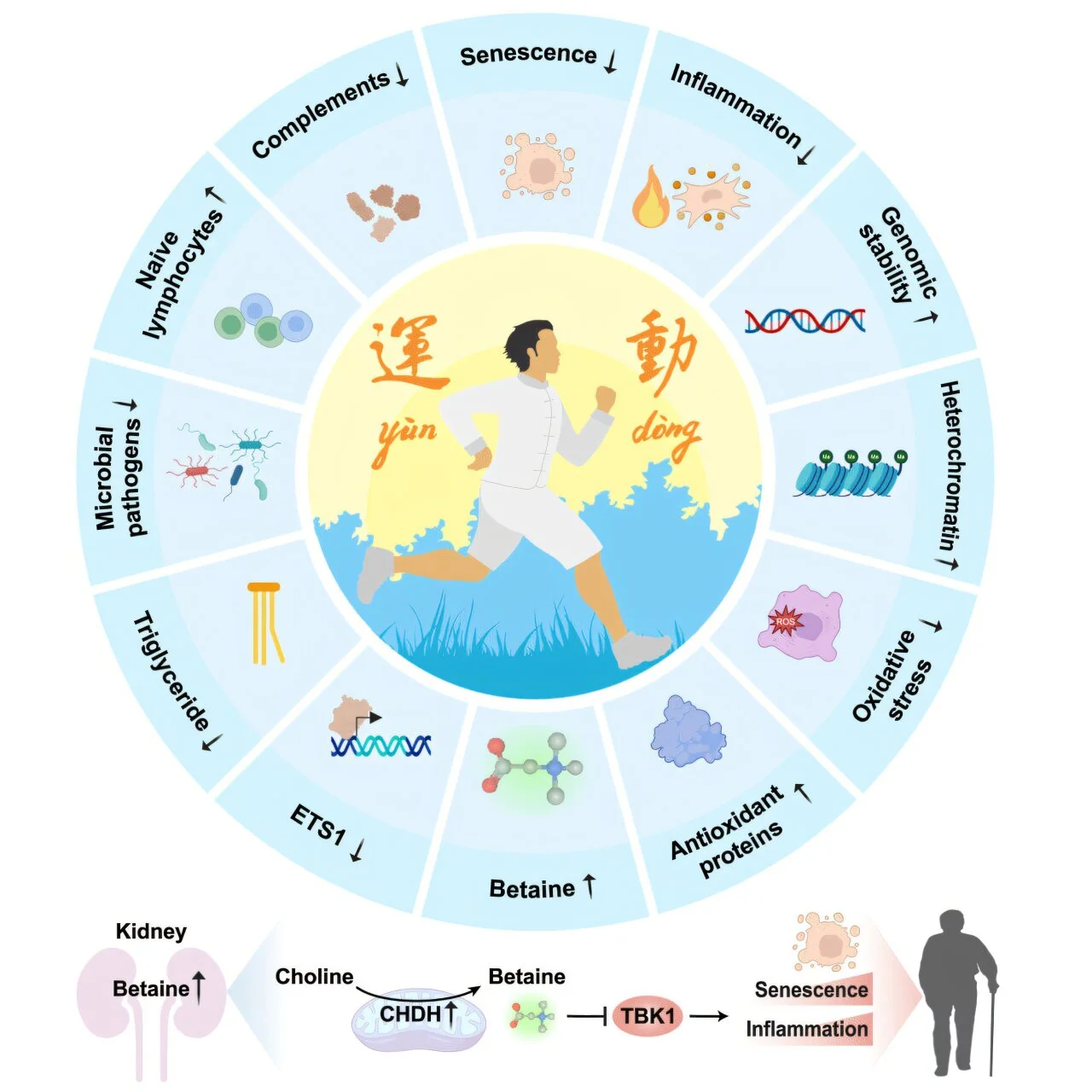
Rest and pacing are essential. Women accustomed to pushing through exhaustion must learn the art of energy management—what patient advocates call “pacing.” This involves carefully balancing activity and rest to avoid triggering setbacks, a strategy particularly important for those with post-exertional malaise, where exertion worsens symptoms.
Rehabilitation programs, especially those focused on respiratory therapy and cardiovascular conditioning, can help rebuild strength. Yet such programs must be tailored—pushing too hard too soon can backfire.
Nutritional support, sleep hygiene, and gentle physical activity like stretching or yoga may aid recovery. Some women find benefit in mindfulness practices, not as cures but as tools for managing the stress and uncertainty of chronic illness.
Importantly, recovery often requires a multidisciplinary approach. Specialists in cardiology, neurology, pulmonology, and mental health may all play roles, coordinated ideally through post-COVID clinics that are emerging in many countries.
When to Seek Care
One of the challenges of Long COVID is knowing when to seek professional help. Persistent symptoms beyond four weeks after infection warrant medical attention, especially if they interfere with daily life. Women should not dismiss ongoing fatigue, chest pain, shortness of breath, palpitations, or neurological changes as “just stress.”
Seek urgent care if symptoms are severe or sudden—for example, chest pain that may indicate heart problems, fainting, or significant breathing difficulties. For ongoing but less acute symptoms, scheduling an evaluation with a primary care physician or a Long COVID clinic can provide guidance, referrals, and validation.
It is also important for women to advocate for themselves in medical settings. Because Long COVID is still poorly understood, symptoms may be minimized. Keeping a detailed symptom diary, bringing support to appointments, and asking directly about Long COVID evaluations can help ensure concerns are taken seriously.
The Role of Support Networks
Recovery is not only medical but also social. Women navigating Long COVID need support from family, friends, workplaces, and communities. This support may take the form of shared caregiving responsibilities, workplace accommodations, or simply acknowledgment of the reality of their illness.
Online support groups have become lifelines, offering spaces where women can share experiences, strategies, and solidarity. The validation of “me too” can be profoundly healing when living with a condition that is often invisible.
Hope from Research and Innovation
Although Long COVID is daunting, research is advancing at unprecedented speed. Scientists are investigating the role of lingering viral fragments, immune system dysregulation, blood clotting abnormalities, and nerve damage. Each discovery brings new avenues for treatment, from antiviral therapies to immune-modulating drugs.
Clinical trials are underway globally, and post-COVID care clinics are expanding access to specialized treatment. The recognition of Long COVID as a legitimate medical condition is itself progress, opening doors to research funding, workplace protections, and disability support.
For women, the growing awareness of gendered differences in Long COVID may lead to more targeted care. Understanding how hormones, immune function, and social roles interact could shape future therapies that address women’s unique needs.
The Human Spirit in the Face of Long COVID
Behind every statistic is a story—a mother learning to pace herself so she can attend her child’s soccer game, a teacher finding new ways to connect with students despite brain fog, a healthcare worker grappling with the irony of becoming a patient herself.
These stories are reminders that Long COVID is not only a medical challenge but also a human one. Women enduring this condition embody resilience: adapting, advocating, and refusing to be silenced. Their voices are crucial in shaping research, policy, and care for the future.
Conclusion: Living Forward
Long COVID may be one of the most profound legacies of the pandemic. For women, its impact is layered—biological vulnerability intersecting with social expectation, personal resilience colliding with systemic gaps in healthcare.
Yet within these challenges lies possibility. The growing global recognition of Long COVID is sparking innovation in medicine and awareness of how chronic illnesses affect lives. Women, as both patients and advocates, are at the forefront of this change.
If you are a woman living with Long COVID, know this: your symptoms are real, your struggle is valid, and your future holds hope. Recovery may be slow, uneven, and frustrating, but it is possible. Seek care, demand support, honor your body’s limits, and trust in the progress of science.
Above all, remember that you are not alone. The story of Long COVID is still being written, and women’s voices are shaping its pages—voices of persistence, of care, of survival, and of determination to reclaim life after illness.