In the long and grinding battle against malaria, where progress has slowed and old strategies are losing ground, scientists have quietly unveiled a promising new weapon. With the precision of a scalpel and the subtlety of nature’s own defenses, two monoclonal antibodies—CIS43LS and L9LS—have emerged from a U.S. research lab as powerful contenders in the fight against one of the world’s deadliest diseases.
Developed by an interdisciplinary team from the Vaccine Research Center in Bethesda, Maryland—a division of the National Institute of Allergy and Infectious Diseases now facing budget uncertainty—these engineered immune molecules have shown remarkable potency in stopping the malaria parasite Plasmodium falciparum at one of its earliest and most vulnerable stages.
The team’s findings, published in Science Translational Medicine, don’t just offer new insight into how antibodies can intercept the parasite. They signal a new chapter in malaria prevention—one where science meets strategy in a war that demands innovation more than ever before.
The Stalemate in the Shadows
For decades, humanity has waged war on malaria with insecticide-treated nets, anti-malarial drugs, and, more recently, vaccines. Yet in many parts of the world—especially across sub-Saharan Africa—those tools are losing their edge. Mosquitoes are adapting. The parasite is evolving. And in the wake of resistance, case numbers are once again creeping upward.
In 2023 alone, the World Health Organization (WHO) estimated 263 million malaria cases worldwide, with 597,000 deaths, most of them among children under five. Yet some estimates, including those from the new study, suggest the death toll could be as high as 700,000 annually.
“Malaria is still a major public health issue, especially in African countries,” said Dr. Neville K. Kisalu, lead author of the study and long-time advocate for broader malaria interventions. “We urgently need new tools.”
And monoclonal antibodies—or mAbs—could be just that.
How Antibodies Work Like Guided Missiles
Antibodies are nature’s defense agents, designed by the immune system to bind to specific invaders. In the lab, scientists can engineer them to target diseases with uncanny precision.
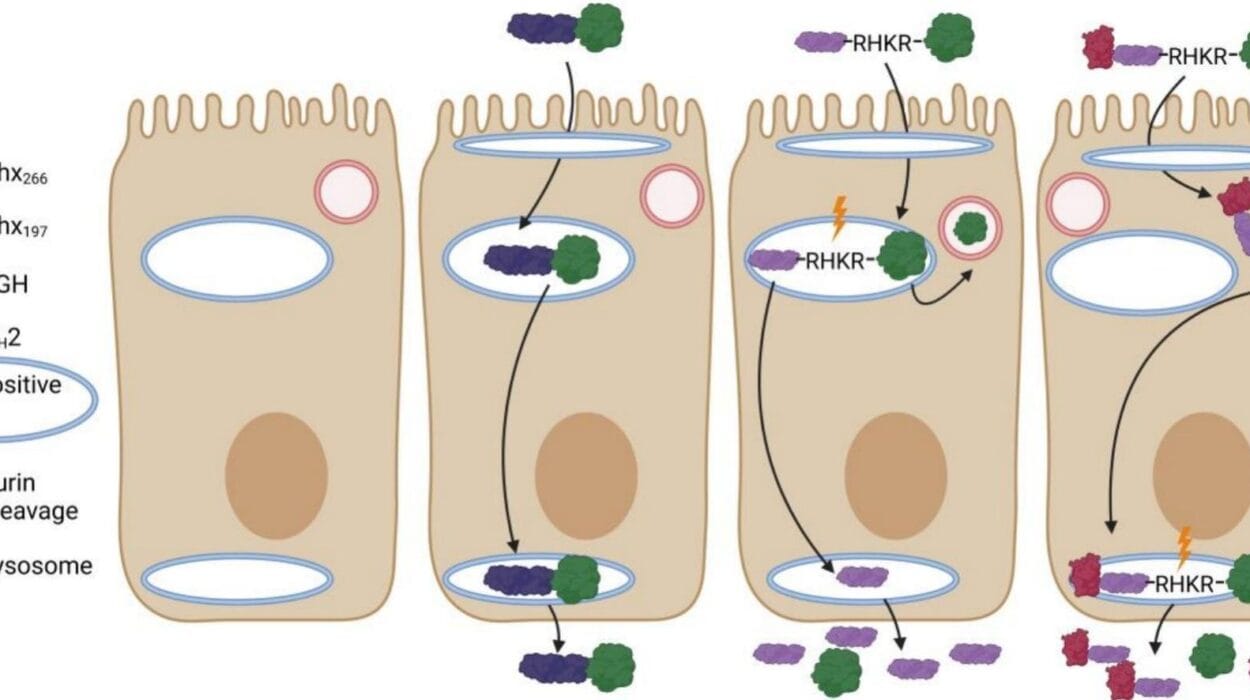
In this study, researchers homed in on a specific surface protein called circumsporozoite protein (PfCSP). This protein coats the sporozoite form of Plasmodium falciparum—a form that enters the human bloodstream after a mosquito bite, and that must invade the liver to replicate and launch a full-blown infection.
By binding to this protein, the monoclonal antibodies CIS43LS and L9LS essentially trap the parasite before it can reach the liver, preventing it from maturing into its deadly forms.
“It’s a window of opportunity,” Kisalu explained. “If we can stop the parasite before it enters the liver, we stop the disease before it even begins.”
Double the Defense, Distinct Approaches
What makes these two antibodies especially exciting is how they work together. They don’t just bind to the same place—they target distinct regions of the PfCSP, creating a double-lock system that’s much harder for the parasite to escape.
Imagine the parasite as a door trying to open into the liver. CIS43LS and L9LS slam down two separate deadbolts. It’s this complementary action that makes the mAbs not only effective, but potentially more resilient against parasite mutation.
And unlike traditional antibody therapies, which often rely on binding to Fc receptors—special docking sites on immune cells—these two antibodies worked independently of that mechanism. That means they could be safer and more flexible in a wider range of patients, including those with immune complications.
Trials in the Lab, With Eyes on the Field
The study was conducted using mouse models, the gold standard for early testing of infectious disease treatments. Both antibodies offered strong protection against malaria in these preclinical trials, even without the help of traditional immune pathways.
But clinical trials in humans have already begun. Early results suggest the same kind of life-saving power: rapid protection after a single dose, long-lasting immunity, and an excellent safety profile.
And perhaps most importantly, mAbs can be administered across all age groups—a vital advantage in regions where malaria doesn’t just strike children, but also lingers in the blood of adults, who unknowingly serve as reservoirs for transmission.
“Adults are the carriers,” Kisalu said. “They may not get sick, but they harbor billions of parasites that mosquitoes can pick up and pass on to others—especially children.”
An Evolving Strategy for a Shifting Enemy
Malaria’s resilience lies in its complexity. The parasite’s life cycle spans 19 different stages, weaving between mosquito and human with astonishing adaptability. The current vaccines—while helpful—don’t block every stage. Monoclonal antibodies could fill that gap, acting as highly targeted shields that stop the infection before it ever gains ground.
Kisalu and his colleagues envision a future where mAbs are part of a layered defense system: vaccines, drugs, mosquito control, and now, precision immunotherapy. And while monoclonal antibodies can be expensive to produce, the team believes engineering more potent versions—with increased binding affinity—could slash costs by requiring smaller doses.
In fact, next-generation antibodies could be two to three times more powerful, opening the door to seasonal use, emergency deployment, or even long-term protection in vulnerable populations.
A Laboratory Disbanded, A Legacy That Lives
Ironically, just as this research is gaining momentum, the Vaccine Research Center that gave it life is facing cutbacks. The team behind the discovery has since scattered, with many moving to other labs across the U.S. and the globe.
But their work endures. And so does the urgency.
Malaria may not make headlines like newer threats, but its toll remains staggering. Every minute, a child dies of a disease we have known how to fight for over a century. Yet with every new mutation, every resistant mosquito, and every under-immunized village, that fight becomes harder.
“Antibodies offer us another path forward,” Kisalu said. “And we’re just beginning to understand their full potential.”
In a world where science often races to keep up with its own breakthroughs, this quiet triumph—two lab-grown molecules, forged in the shadows of budget cuts and disease fatigue—might just represent the most hopeful development in malaria treatment in a generation.
Reference: Neville K. Kisalu et al, FcγR binding differentially contributes to protection by two human monoclonal antibodies targeting Plasmodium falciparum circumsporozoite protein, Science Translational Medicine (2025). DOI: 10.1126/scitranslmed.adk6745