Cancer has long stood as one of humanity’s most formidable biological adversaries. It is not a single disease, but a vast constellation of disorders driven by genetic mutations, cellular miscommunication, and complex interactions between the body and its environment. For decades, cancer treatment advanced through incremental progress: improved chemotherapy drugs, refined surgical techniques, and targeted radiation. Yet by 2025, a profound transformation is underway. Artificial intelligence is no longer a distant promise or experimental novelty. It has become an active force reshaping how cancer is detected, understood, and treated.
The revolution driven by AI in oncology is not defined by a single breakthrough, but by a quiet convergence of data, algorithms, and clinical practice. AI systems now analyze medical images with superhuman consistency, sift through genomic data at a scale impossible for human experts, and help clinicians tailor therapies to the unique biological profile of each patient. This transformation is altering not only outcomes, but also the emotional experience of cancer care, replacing uncertainty with clarity and generalized treatment with precision.
The Data-Driven Nature of Cancer and the Rise of AI
Cancer is fundamentally a disease of information. At its core lie changes in DNA, disruptions in gene regulation, and altered cellular signaling pathways. Each tumor carries a biological story written in genetic code, protein expression, and tissue structure. Historically, clinicians could read only fragments of this story. By 2025, AI has emerged as the essential interpreter of cancer’s complexity.
Modern oncology generates enormous volumes of data. Medical imaging produces detailed visual records of tumors. Genomic sequencing reveals millions of data points from a single patient’s DNA. Electronic health records capture treatment histories, responses, and side effects across populations. AI thrives in precisely this environment. Machine learning algorithms are designed to detect patterns within vast, multidimensional datasets, uncovering relationships that are invisible to traditional statistical methods.
This capacity allows AI to move cancer care beyond averages. Instead of asking how most patients respond to a treatment, AI systems analyze how a specific patient, with a specific tumor biology and medical history, is likely to respond. This shift marks a foundational change in oncology, from population-based medicine to truly individualized care.
AI in Early Cancer Detection and Diagnosis
Early detection remains one of the most powerful determinants of cancer survival. Cancers identified at an early stage are often more treatable, less aggressive, and associated with significantly better outcomes. In 2025, AI plays a decisive role in identifying cancer earlier and more accurately than ever before.
Medical imaging lies at the heart of this transformation. AI systems trained on millions of radiological images can detect subtle abnormalities in mammograms, CT scans, MRIs, and pathology slides. These algorithms do not tire, lose concentration, or overlook rare patterns. They identify minute changes in tissue structure that may signal the earliest stages of malignancy, often before symptoms appear.
Importantly, AI does not replace radiologists or pathologists. Instead, it functions as an intelligent partner. By highlighting areas of concern and providing probability-based assessments, AI enhances human expertise. This collaboration reduces diagnostic errors, shortens the time to diagnosis, and alleviates the emotional burden on patients waiting for results. For many individuals, the difference between early and late diagnosis is the difference between curative treatment and long-term management.
Transforming Pathology Through Computational Insight
Pathology has traditionally relied on the trained human eye examining tissue samples under a microscope. While highly skilled, this approach is inherently subjective and limited by human perception. By 2025, AI-powered computational pathology has reshaped this foundational discipline.
Digital pathology enables tissue slides to be scanned into high-resolution images that AI algorithms can analyze pixel by pixel. These systems quantify features such as cell shape, spatial organization, and molecular markers with extraordinary precision. They can distinguish between aggressive and indolent tumors, predict the likelihood of metastasis, and estimate how a tumor may respond to specific therapies.
This quantitative approach brings consistency and reproducibility to cancer diagnosis. Two pathologists examining the same sample may reach slightly different conclusions, but an AI system applies the same criteria every time. This consistency improves confidence in diagnoses and ensures that treatment decisions are based on the most accurate possible information.
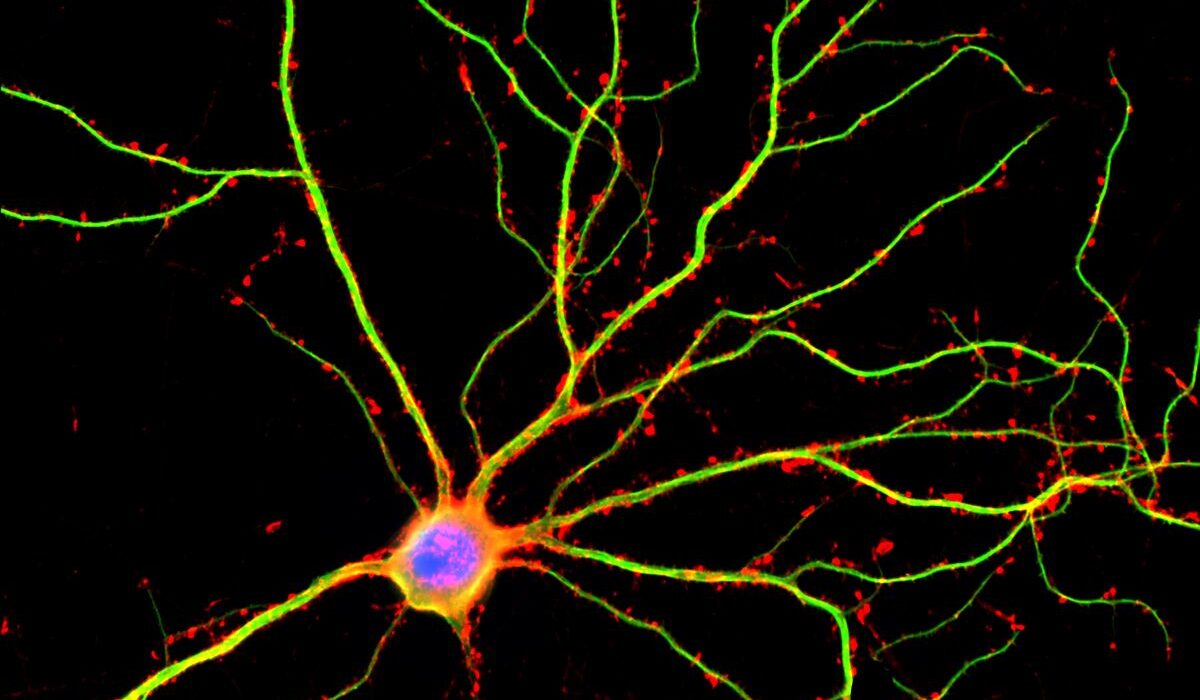
Genomics, AI, and the Molecular Understanding of Cancer
The genetic revolution in oncology has revealed that cancer is driven by specific mutations and molecular pathways. However, interpreting genomic data is extraordinarily complex. A single tumor genome may contain thousands of mutations, many of uncertain significance. In 2025, AI serves as the indispensable guide through this molecular labyrinth.
Machine learning models analyze genomic sequences to identify driver mutations that actively promote cancer growth, distinguishing them from harmless passenger mutations. These systems integrate genomic data with clinical outcomes, learning which genetic patterns are associated with treatment response or resistance. This knowledge enables oncologists to select targeted therapies designed to interrupt the precise molecular mechanisms fueling a patient’s cancer.
AI also accelerates the discovery of new cancer subtypes. By clustering tumors based on molecular similarity rather than tissue of origin alone, AI reveals hidden biological categories. These insights lead to more refined diagnoses and open the door to therapies tailored to previously unrecognized patient groups.
Personalized Treatment Planning and Precision Oncology
One of the most profound impacts of AI in 2025 is its role in personalizing cancer treatment. Traditional oncology often followed standardized protocols, guided by tumor type and stage. While effective for many patients, this approach could not account for individual biological variability. AI changes this paradigm.
By integrating data from imaging, genomics, pathology, and patient history, AI systems generate personalized treatment recommendations. These models estimate the likelihood that a patient will benefit from chemotherapy, immunotherapy, targeted drugs, or combinations thereof. They also predict potential side effects, enabling clinicians to balance efficacy with quality of life.
This personalized approach is especially transformative for patients with advanced or rare cancers, where treatment decisions are often uncertain. AI provides evidence-based guidance in situations where clinical experience alone may be insufficient, offering patients options grounded in data rather than guesswork.
AI and the Evolution of Immunotherapy
Immunotherapy has emerged as one of the most promising cancer treatments of the 21st century, harnessing the immune system to recognize and destroy cancer cells. Yet not all patients benefit from immunotherapy, and predicting response has been a major challenge. In 2025, AI plays a critical role in unlocking the full potential of these therapies.
AI models analyze tumor microenvironments, immune cell populations, and molecular markers to identify patients most likely to respond to immunotherapy. They detect subtle patterns in gene expression and protein signaling that indicate whether a tumor can be recognized by the immune system. This precision reduces unnecessary exposure to treatments that may be ineffective or cause significant side effects.
Furthermore, AI helps design personalized cancer vaccines and cell-based therapies. By identifying tumor-specific antigens unique to an individual’s cancer, AI-guided approaches enable highly targeted immune responses. This represents a new frontier in oncology, where treatment is not only personalized, but biologically bespoke.
Optimizing Radiation Therapy with AI
Radiation therapy is a cornerstone of cancer treatment, but it requires exquisite precision. Delivering sufficient radiation to destroy tumors while sparing healthy tissue is a complex technical challenge. In 2025, AI enhances every stage of radiation therapy planning and delivery.
AI algorithms analyze imaging data to delineate tumor boundaries with unprecedented accuracy. They model how radiation beams interact with different tissues, optimizing dose distribution in three dimensions. During treatment, AI systems monitor patient movement and anatomical changes, adjusting radiation delivery in real time.
These advances reduce side effects, shorten treatment courses, and improve tumor control. For patients, this means fewer complications and a treatment experience that is not only more effective, but also more humane.
Accelerating Drug Discovery and Clinical Trials
The development of new cancer drugs has historically been slow, expensive, and uncertain. AI is dramatically accelerating this process by transforming how drugs are discovered and tested. By 2025, AI-driven drug discovery has become a central pillar of oncology research.
Machine learning models analyze chemical structures, biological targets, and experimental data to predict which compounds are most likely to be effective against specific cancer pathways. This approach reduces reliance on trial-and-error experimentation, focusing resources on the most promising candidates.
AI also reshapes clinical trials. By analyzing patient data, AI helps identify individuals most likely to benefit from experimental therapies, increasing trial efficiency and success rates. Adaptive trial designs guided by AI enable real-time adjustments based on emerging results, accelerating the translation of discoveries into clinical practice.
Monitoring Treatment Response and Disease Progression
Cancer treatment does not end with therapy selection. Continuous monitoring is essential to assess response, detect recurrence, and adapt strategies as tumors evolve. In 2025, AI enables dynamic, real-time cancer management.
AI systems analyze follow-up imaging, blood-based biomarkers, and clinical data to detect early signs of treatment success or failure. Liquid biopsies, which identify tumor DNA fragments circulating in the blood, generate complex datasets that AI interprets with high sensitivity. These tools allow clinicians to detect recurrence months earlier than traditional methods.
This proactive approach transforms cancer from a reactive disease to a monitored condition. Patients benefit from timely interventions, reduced anxiety, and a sense that their care is continuously informed by the latest data.
AI, Ethics, and the Human Dimension of Cancer Care
The integration of AI into cancer treatment raises important ethical and human considerations. In 2025, these questions are no longer theoretical. Issues of data privacy, algorithmic transparency, and equitable access demand careful attention.
AI systems learn from patient data, making robust data governance essential. Ensuring that models are trained on diverse populations is critical to avoid biases that could exacerbate health disparities. Transparency in AI decision-making builds trust, enabling clinicians and patients to understand how recommendations are generated.
Crucially, AI does not replace the human relationship at the heart of cancer care. Compassion, empathy, and communication remain irreplaceable. AI enhances decision-making, but it is clinicians who guide patients through fear, hope, and uncertainty. When used responsibly, AI allows healthcare professionals to spend less time on administrative tasks and more time on meaningful human interaction.
The Emotional Impact of AI-Driven Oncology
Beyond clinical metrics, AI profoundly affects the emotional landscape of cancer treatment. For patients, uncertainty is often the most distressing aspect of the disease. AI reduces this uncertainty by providing clearer diagnoses, more accurate prognoses, and tailored treatment plans.
Knowing that decisions are informed by vast bodies of data can offer reassurance during an emotionally overwhelming journey. For clinicians, AI alleviates cognitive burden, enabling them to focus on patient care rather than data overload. This emotional relief has tangible effects on well-being, burnout, and the overall quality of care.
In this sense, AI’s contribution is not only technological, but deeply human. It reshapes the experience of cancer treatment, making it more informed, more responsive, and more compassionate.
Challenges and Limitations of AI in Cancer Treatment
Despite its transformative potential, AI is not a panacea. In 2025, significant challenges remain. AI models depend on data quality, and incomplete or biased datasets can lead to flawed conclusions. Integrating AI tools into clinical workflows requires training, infrastructure, and cultural change.
Interpretability remains a central issue. Some AI systems function as complex “black boxes,” making it difficult to explain their recommendations in intuitive terms. Addressing this limitation is essential for clinical trust and regulatory approval.
Moreover, access to AI-driven cancer care is uneven across regions and healthcare systems. Ensuring that these advances benefit all patients, not only those in well-resourced settings, is a moral and public health imperative.
The Future Trajectory of AI in Oncology
By 2025, AI has already reshaped cancer treatment, yet its full potential is still unfolding. Future developments aim to integrate multi-omics data, real-world evidence, and longitudinal patient monitoring into unified AI platforms. These systems will not only treat cancer, but anticipate it, identifying risk years before disease develops.
The long-term vision of AI in oncology is predictive, preventive, and personalized medicine. Cancer may increasingly be managed as a chronic condition, detected early, treated precisely, and monitored continuously. While challenges remain, the trajectory is clear: AI is redefining what is possible in cancer care.
Conclusion: A New Era in the Fight Against Cancer
In 2025, artificial intelligence stands as one of the most powerful allies humanity has ever wielded against cancer. It does not offer miracles or guarantees, but it provides clarity where there was confusion, precision where there was generalization, and hope where there was uncertainty. Through data-driven insight and human-centered application, AI transforms cancer treatment into a more intelligent, responsive, and compassionate endeavor.
This revolution is not about machines replacing doctors or algorithms overshadowing human judgment. It is about expanding our capacity to understand a complex disease and respond with wisdom and care. In the ongoing struggle against cancer, AI represents a turning point, not an end, but a profound beginning in how we confront one of life’s greatest challenges.