Hidradenitis suppurativa (HS) is a skin condition that goes far beyond ordinary breakouts. It brings with it painful lumps, draining lesions, and deep inflammation in sensitive areas like the armpits, groin, and buttocks. For the people who live with it, HS can mean constant discomfort, restricted movement, emotional distress, and in many cases, stigma.
Despite growing awareness, effective treatment remains a major challenge. Standard therapies such as antibiotics or biologic drugs can help, but many patients find their relief partial or short-lived. For those who also carry the heavy burden of obesity—a majority of HS patients do—the cycle of inflammation, weight gain, and disease progression becomes especially hard to break.
Why Obesity Matters in HS
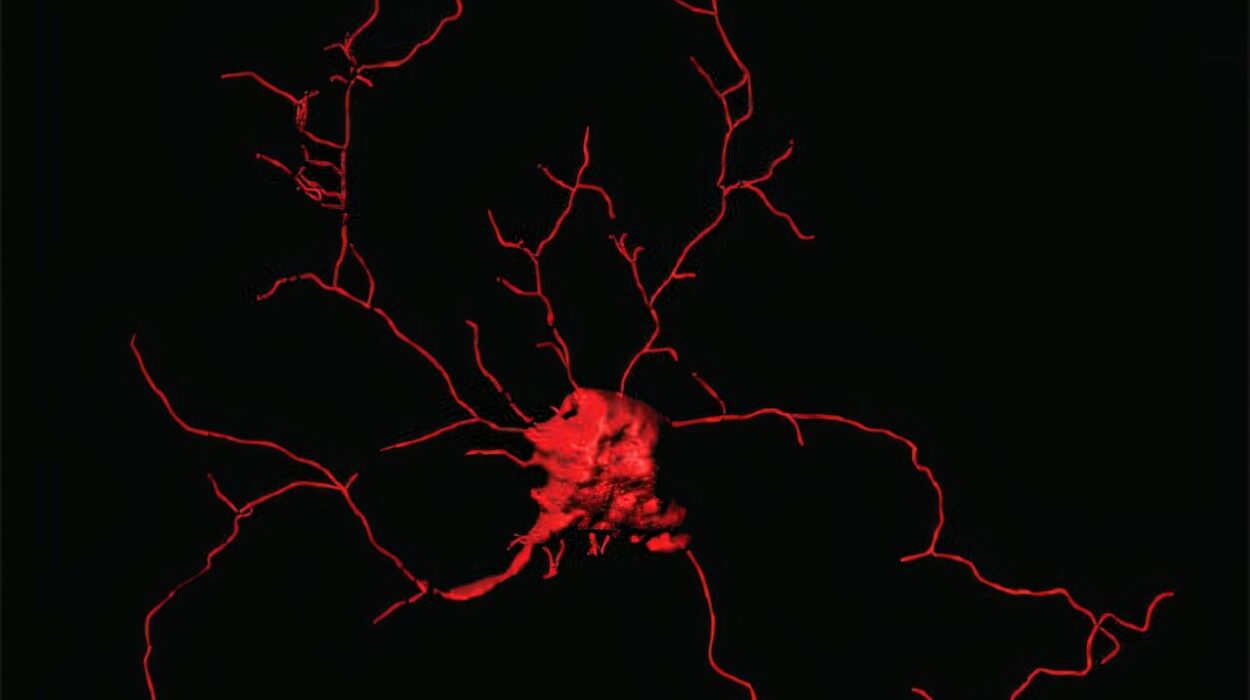
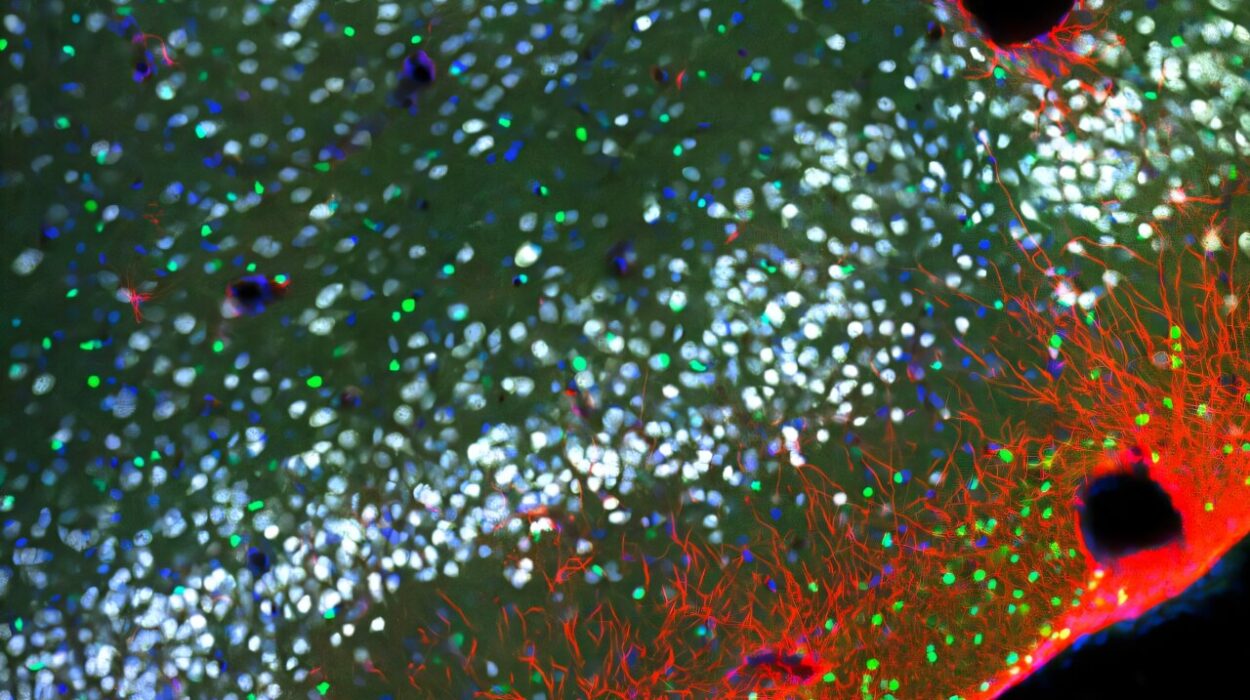
HS is more than just a skin problem. Beneath the painful nodules lies a complex story of immune imbalance, inflammation, and metabolic dysfunction. Fat tissue in people with obesity doesn’t just store energy—it becomes an active player in disease, producing molecules that fuel inflammation and disrupt normal immune function.
This creates a vicious cycle: inflamed fat tissue worsens HS, and the painful condition often makes physical activity harder, contributing to weight gain. Studies have shown that when patients with HS lose weight, either through diet or bariatric surgery, their symptoms often improve. But significant weight loss is difficult to achieve and even harder to maintain.
This is where an unexpected class of medications enters the picture—drugs originally developed not for skin disease, but for diabetes.
From Blood Sugar to Body Weight: The Rise of GLP-1 Receptor Agonists
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are a relatively new family of drugs that first transformed the treatment of type 2 diabetes. They mimic a natural hormone in the body that helps regulate blood sugar and appetite. The results have been striking: not only do GLP-1 RAs control glucose levels, but they also lead to substantial weight loss.
In recent years, drugs like semaglutide and liraglutide have gained global attention for their weight-reducing power, offering patients a tool that goes beyond dieting alone. Yet researchers began to wonder: could their benefits extend even further? Could these medications, by dampening inflammation and reducing body fat, also help conditions like HS?
The French Study That Sparked Hope
A multicenter study led by Rennes University Hospital in France, published in JAMA Dermatology, set out to answer that very question. The researchers looked back at real-world data from 66 adults with HS who were prescribed GLP-1 receptor agonists—semaglutide, dulaglutide, or liraglutide—for at least three months.
The group was typical of many HS patients: the median age was 46, most were women, and nearly all (86%) also had diabetes. Their median body mass index (BMI) was 39.4, placing them firmly in the obesity range. More than half were already on other treatments for HS when they started the GLP-1 medication.
The researchers followed these patients for a median of 18.5 months, tracking changes at six months and again at their last consultation.
What the Study Found
The results painted a cautiously optimistic picture. By six months, just over half (54%) of patients saw measurable improvements in their HS. About one in ten experienced a dramatic two-point or greater improvement on the HS Physician’s Global Assessment scale, a standard tool for grading disease severity.
By the final follow-up, the numbers looked even stronger. Nearly two-thirds (62%) showed improvements, with about a third reaching that significant two-point threshold. Two out of three patients reported fewer flare-ups, and 60% experienced reduced pain—an outcome that can dramatically improve quality of life.
These findings suggest that GLP-1 receptor agonists may not only help with weight loss, but may directly impact HS activity itself.
Why Might These Drugs Work for HS?
The exact reasons for the improvements are still being investigated, but scientists have several compelling theories.
One explanation is straightforward: weight loss reduces the inflammatory burden of obesity. With less fat tissue releasing pro-inflammatory molecules, the body’s immune system may calm down, leading to fewer HS flares.
But there could be more going on. GLP-1 receptor agonists may have their own anti-inflammatory effects independent of weight loss. Studies suggest they can lower certain inflammatory cytokines and even temper the body’s overreaction to bacterial triggers, which are thought to play a role in HS lesions. They may also help with tissue healing by reducing enzymes that break down the skin’s structural framework.
If true, these effects could mean that GLP-1 receptor agonists might benefit HS patients even if they are not overweight—a tantalizing possibility for future research.
A Step Forward, But Not Yet a Cure
The French study offers hope, but it also has limitations. It was retrospective, meaning researchers looked back at existing data rather than conducting a randomized controlled trial. Without a comparison group, it’s difficult to know how much of the improvement was due to the drugs themselves versus other factors, such as concurrent treatments or natural fluctuations in disease activity.
Still, the consistent pattern across multiple centers and dozens of patients suggests the signal is real and worth pursuing. Randomized trials will be crucial to confirm whether GLP-1 receptor agonists should become part of standard care for HS.
What This Means for Patients
For people living with HS, these findings carry both hope and caution. Hope, because a new class of drugs already widely available for diabetes and weight loss might also help ease their painful condition. Caution, because more research is needed before doctors can confidently prescribe these medications specifically for HS.
Patients considering this approach should speak with their healthcare providers. GLP-1 receptor agonists can be powerful tools, but they also carry potential side effects such as nausea, gastrointestinal discomfort, and rare risks that need medical oversight.
Looking Ahead
Hidradenitis suppurativa has long been a frustrating condition with too few effective options. The discovery that diabetes drugs might improve HS is a reminder of how interconnected the body truly is—how hormones, fat tissue, immune responses, and the skin’s health all intertwine.
For now, the story of GLP-1 receptor agonists and HS is just beginning. But if future trials confirm their promise, these drugs may open a new chapter of hope for thousands living with this painful condition.
More information: Louise Gouvrion et al, Glucagon-Like Peptide-1 Receptor Agonists in Hidradenitis Suppurativa, JAMA Dermatology (2025). DOI: 10.1001/jamadermatol.2025.2723