Women’s health is often spoken of in whispers—tucked into small conversations between friends, covered with nervous laughter, or postponed until discomfort becomes unbearable. Yet, the truth is that every woman deserves to understand her body, to feel empowered about her health, and to know when to seek medical help without shame or hesitation. The gynecologist’s office, for many, is a place of both anxiety and reassurance. It is where intimate concerns meet scientific care, where prevention saves lives, and where silence can turn into solutions.
But here’s the reality: many women delay or avoid seeing a gynecologist. Sometimes it’s fear, sometimes embarrassment, sometimes the belief that “it’s not serious enough.” And sometimes, it’s simply not knowing when a visit is necessary. This delay can come at a cost, because gynecologists do not only treat emergencies—they are partners in maintaining lifelong reproductive, sexual, and overall health.
Understanding when to schedule a routine visit, and recognizing red flags that should never be ignored, is not just medical advice—it is self-preservation, self-respect, and self-love.
Why Gynecology Matters Beyond Reproduction
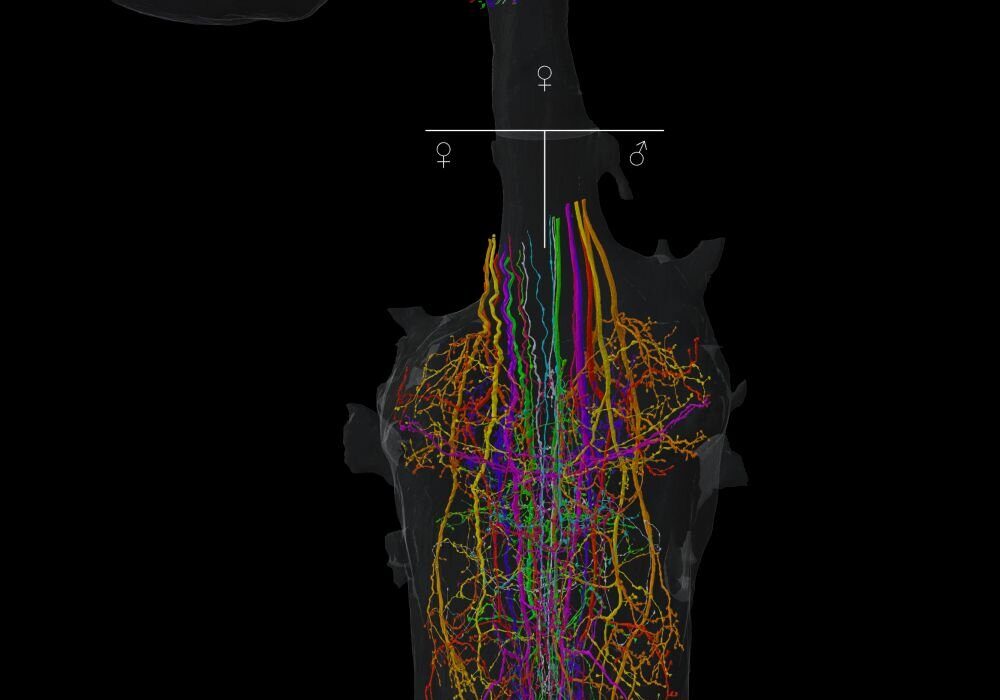
Many people think of gynecology as being solely about pregnancy or childbirth. While it certainly covers those areas, it extends far beyond. Gynecology focuses on the health of the female reproductive system, but because hormones, menstrual cycles, and reproductive organs influence overall well-being, gynecology is deeply connected to general health too.
From adolescence through post-menopause, the gynecologist becomes a guide through the transitions of womanhood. Whether it’s navigating the first period, managing painful cycles, planning for pregnancy, detecting infections, addressing fertility issues, or easing the changes of menopause, gynecology is not just about treatment—it is about understanding.
Seeing a gynecologist regularly allows women to catch silent health issues early, manage chronic conditions more effectively, and receive preventive care that can change the course of their lives.
The Role of Routine Gynecological Visits
Routine visits are not a luxury; they are a necessity. Even when no symptoms are present, regular check-ups create a baseline of health and catch concerns that may otherwise remain hidden. A routine visit may include a physical exam, pelvic exam, Pap smear, breast exam, or discussions about contraception, menstruation, sexuality, or menopause.
These visits often serve as a safe space to ask questions that might feel too personal or awkward elsewhere. From irregular bleeding to questions about sexual discomfort, the gynecologist’s office is where these issues can be addressed with compassion and evidence-based answers.
But how often should one go? Most experts recommend an annual visit, though the exact frequency may depend on age, personal health history, and risk factors. The important thing is consistency—making sure preventive care is not neglected.
Red Flags That Should Never Be Ignored
While routine visits are the foundation, there are also urgent warning signs—red flags—that demand immediate attention. Ignoring them can allow minor issues to escalate into major health threats. These symptoms are the body’s way of signaling that something is wrong and should never be dismissed as “normal” or “just stress.”
Abnormal Bleeding
One of the most common and concerning reasons to see a gynecologist is unusual vaginal bleeding. This includes:
- Bleeding between periods
- Very heavy menstrual flow requiring frequent pad or tampon changes
- Bleeding after sex
- Bleeding after menopause
Abnormal bleeding can be linked to conditions ranging from hormonal imbalances and fibroids to infections and, in rare cases, cancers of the uterus or cervix.
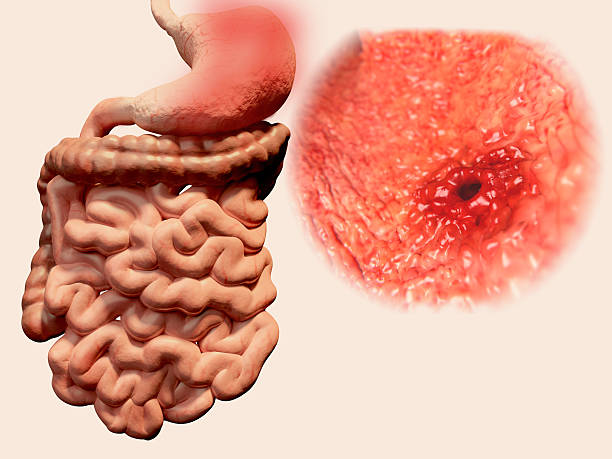
Severe Pelvic Pain
Menstrual cramps are often considered “normal,” but pain that interferes with daily life, is severe, or occurs outside the menstrual cycle should not be ignored. Pelvic pain may signal endometriosis, pelvic inflammatory disease, ovarian cysts, or even ectopic pregnancy.
Unusual Vaginal Discharge or Odor
Some vaginal discharge is healthy and natural, but sudden changes in color, consistency, or smell may point to infections, including bacterial vaginosis, yeast infections, or sexually transmitted infections (STIs). Early diagnosis prevents complications and transmission.
Pain During Intercourse
Sex should not be painful. If it is, it may indicate underlying conditions such as vaginal dryness, infections, pelvic floor disorders, or endometriosis. Emotional health and relationship dynamics may also be intertwined with physical discomfort, making this an important topic to address openly with a gynecologist.
Lumps, Bumps, or Breast Changes
Changes in breast tissue, whether lumps, persistent pain, or unusual discharge from the nipple, should always be evaluated. While many changes are benign, they can sometimes signal breast cancer or other serious conditions.
Missed or Irregular Periods
Occasional irregularity can be due to stress or lifestyle changes, but consistent absence or erratic cycles may reflect thyroid problems, polycystic ovary syndrome (PCOS), or hormonal imbalances. For women who are sexually active, missed periods can also indicate pregnancy or early miscarriage.
Painful or Frequent Urination
Symptoms like burning during urination, urgency, or frequent trips to the bathroom may signal urinary tract infections or other urological concerns. When combined with pelvic pain, they can indicate more complex gynecological conditions.
Signs of Menopause Complications
For women in their 40s or 50s, menopause brings natural changes, but excessive hot flashes, severe mood swings, bone pain, or postmenopausal bleeding require evaluation. These may reflect complications that need medical management.
The Routine Visit Checklist
A routine gynecological visit is not just a physical examination—it is a dialogue, a partnership, and an opportunity to create a comprehensive picture of health. While every appointment may vary depending on age, history, and needs, there are key components that typically form the backbone of preventive care.
The Medical History Conversation
Before any physical examination, the gynecologist will ask questions about medical history, menstrual cycle patterns, sexual activity, contraception, pregnancies, family health history, and current symptoms. This conversation sets the stage for tailored care and helps uncover hidden risk factors.
The Physical and Pelvic Exam
A physical exam often includes checking vital signs, breast examination, and sometimes a pelvic exam. During the pelvic exam, the doctor assesses the health of the uterus, ovaries, and vagina. While this may feel uncomfortable, it is typically quick and can reveal early signs of conditions like fibroids or infections.
The Pap Smear
The Pap smear is one of the most effective preventive tests in modern medicine. It involves collecting cells from the cervix to detect changes that may signal cervical cancer or precancerous lesions. For many women, it is recommended every three years (or more frequently depending on risk).
Breast Health Evaluation
Depending on age and family history, breast exams or referrals for mammograms may be part of routine care. Breast cancer, when caught early, is highly treatable, making these screenings critical.
Conversations About Contraception and Sexual Health
Routine visits are the ideal time to discuss birth control options, sexual satisfaction, STI prevention, or questions about libido. These conversations ensure reproductive autonomy and overall well-being.
Fertility and Family Planning
For women planning to conceive—or struggling to do so—routine visits provide guidance. Fertility evaluations, preconception counseling, and discussions about pregnancy health can all be part of the checklist.
Menstrual Health Review
Menstruation is often overlooked as a “routine” aspect of life, but its patterns reveal a great deal about hormonal balance and reproductive health. Tracking cycles, noting irregularities, and discussing discomfort help gynecologists identify conditions like PCOS or endometriosis.
Gynecology Across Life Stages
The reasons for visiting a gynecologist evolve throughout life. A teenager may need guidance about menstrual health and safe sexual practices. A woman in her 20s may be more focused on contraception and STI prevention. In her 30s, family planning and fertility may take center stage. In her 40s and 50s, perimenopause and menopause raise new challenges. Even in later years, gynecology remains important for maintaining pelvic health, sexual wellness, and cancer screenings.
Biology and hormones shift with age, but the need for gynecological care never disappears. This continuity underscores the role of gynecology as a lifelong ally.
Breaking Barriers: Fear, Shame, and Misconceptions
For many women, visiting a gynecologist is associated with anxiety. Some worry about pain during exams, others fear judgment, and many simply feel embarrassed discussing intimate issues. Cultural taboos and lack of awareness often deepen the reluctance.
Yet, these barriers can be broken with education, empathy, and trust. Gynecologists are trained not only to diagnose but also to listen. The more openly patients communicate, the more effective the care becomes. Creating a culture where women speak about reproductive health as openly as they do about dental or eye health is essential to breaking cycles of neglect.
The Emotional Dimension of Gynecology
Gynecology is not just about bodies—it is also about emotions. Menstrual disorders can impact mental health, fertility struggles can bring grief, menopause can spark anxiety, and sexual dysfunction can affect relationships. Gynecological care must therefore address both the physical and psychological dimensions of women’s health.
When a woman feels heard, respected, and supported, the gynecologist’s office becomes more than a clinic—it becomes a sanctuary where healing begins.
Preventive Care as Empowerment
Too often, women only visit the gynecologist when something is wrong. But the true power of gynecology lies in prevention. Screenings catch silent diseases before they progress. Vaccinations, like the HPV vaccine, prevent future cancers. Counseling offers tools for healthier choices.
Preventive care is not about fear—it is about empowerment. It is a way for women to take charge of their health, ensuring that small issues don’t grow into life-altering challenges.
When in Doubt, Check It Out
A guiding principle for women’s health is simple: when in doubt, check it out. If something feels different, unusual, or worrisome, it is always worth seeking medical advice. Waiting often increases anxiety and risks. The gynecologist is there not only to treat but also to reassure.
Even if the concern turns out to be minor, the peace of mind gained is invaluable. And if the concern is serious, early action can make all the difference.
Conclusion: Listening to the Language of the Body
The female body speaks in its own language—through cycles, symptoms, and sensations. Gynecology teaches us to listen, interpret, and respond. Routine visits maintain the foundation, while attention to red flags protects against crises.
Seeing a gynecologist is not an act of fear; it is an act of courage and care. It is saying: My health matters. My body matters. My future matters.
In a world where women’s health is too often overlooked, neglected, or silenced, prioritizing gynecological care becomes both a personal responsibility and a collective statement. The question is not just when to see a gynecologist—it is whether we are willing to honor our health enough to make that visit.
Because the truth is simple: every woman deserves the right to health, dignity, and a life where her body’s whispers are heard before they become cries.