A sudden burning sensation, the relentless urge to urinate, the discomfort that lingers long after you’ve left the bathroom—if you’ve ever had a urinary tract infection (UTI), you know the unique kind of misery it brings. For women especially, UTIs are a common yet deeply disruptive condition. They can turn ordinary days into exhausting struggles, and repeated infections can weigh heavily on both physical health and emotional well-being.
Yet, there is hope. UTIs are preventable, manageable, and treatable. With the right knowledge, women can protect themselves, find fast relief when symptoms arise, and reduce the risk of recurrence. This guide is a deep dive into the world of UTIs: what causes them, how they can be prevented, and the most effective ways to find relief when they strike. It is both practical and compassionate, designed not just to share medical facts but also to provide reassurance that you are not alone in this journey.
What Exactly Is a UTI?
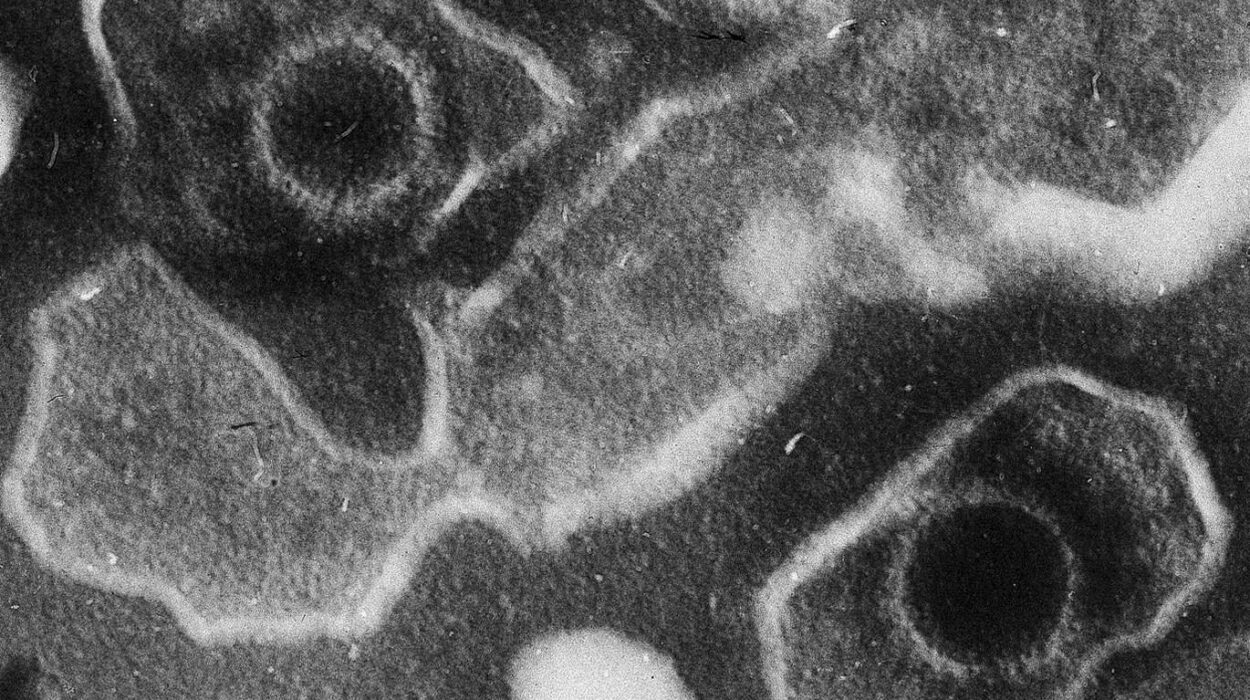
A urinary tract infection occurs when harmful bacteria—most commonly Escherichia coli (E. coli)—invade the urinary system. The urinary tract includes the kidneys, ureters, bladder, and urethra. While UTIs can occur in any of these areas, most infections develop in the bladder, a condition known as cystitis. When bacteria reach the kidneys, the infection becomes more severe and potentially dangerous.
For women, the risk is much higher than for men. The female urethra is shorter and closer to the anus, making it easier for bacteria to travel into the bladder. Statistics reveal that nearly 50–60% of women will experience at least one UTI in their lifetime, and many face recurrent infections.
The Emotional Burden of UTIs
While the physical symptoms of UTIs are well-documented—burning, urgency, cloudy or bloody urine—what often goes unspoken is the emotional toll. Women frequently describe feeling embarrassed, frustrated, or anxious. Recurrent UTIs can create fear of intimacy, affect work productivity, and even disrupt sleep. The unpredictability of when the next infection might strike adds to this burden.
Biology explains the vulnerability, but compassion reminds us that UTIs are not a personal failing. They are a common health challenge, and by acknowledging both the science and the human experience, we can better address them.
How UTIs Develop
The development of a UTI is both simple and complex. Most begin when bacteria from the gastrointestinal tract—particularly E. coli—find their way to the urethra. Once there, they can adhere to the lining of the urinary tract and multiply. Normally, the body has defenses in place: urine flow helps flush bacteria out, and the immune system fights infections. But when these defenses are overwhelmed or compromised, infection takes hold.
Factors that increase the risk include:
- Sexual activity, which can introduce bacteria into the urethra.
- Hormonal changes, particularly during menopause, which reduce protective vaginal flora.
- Use of certain contraceptives like diaphragms or spermicides.
- A weakened immune system or conditions like diabetes.
- Poor hydration, leading to infrequent urination.
Though UTIs are common, each woman’s experience is unique. Some may develop infections only occasionally, while others struggle with frequent recurrences despite careful hygiene and prevention.
The Role of Hydration
One of the simplest yet most effective ways to prevent and manage UTIs is through hydration. Water is not just a life-sustaining fluid; it is a natural cleanser for the urinary tract. When you drink enough water, you increase urine output, which helps flush out bacteria before they can establish an infection.
Research consistently shows that women who increase their water intake experience fewer UTIs. In fact, one clinical trial demonstrated that women prone to recurrent UTIs reduced their infection rates significantly by simply drinking an additional 1.5 liters of water daily.
Hydration is more than just gulping down water when you’re thirsty. It is about creating a consistent habit—keeping a water bottle nearby, sipping throughout the day, and paying attention to the color of your urine. Pale yellow usually indicates good hydration, while darker shades suggest it’s time to drink more.
Hygiene and Everyday Practices
Hygiene plays a crucial role in UTI prevention, though it is often misunderstood. Overly aggressive cleaning can disrupt the body’s natural balance, while inadequate hygiene can allow bacteria to thrive. The key lies in gentle, consistent practices.
Wiping from front to back, urinating after sexual intercourse, and avoiding irritating products like scented sprays or douches are practical habits that reduce risk. Cotton underwear and breathable fabrics help keep the genital area dry, minimizing bacterial growth.
However, it’s important to recognize that even with perfect hygiene, UTIs can still occur. Women should never feel guilty or ashamed when infections happen. Hygiene reduces risk but does not guarantee immunity.
Nutrition and the Role of Diet
Food and nutrition can support urinary health in subtle yet powerful ways. A balanced diet that strengthens the immune system can reduce susceptibility to infections. But beyond general health, certain foods and compounds directly influence urinary tract defenses.
Cranberries are perhaps the most famous example. Compounds in cranberries, particularly proanthocyanidins, may prevent bacteria from adhering to the bladder wall. While cranberry juice has long been promoted, modern research suggests that concentrated cranberry supplements are more effective, as juices are often diluted and loaded with sugar.
Probiotics, found in yogurt, kefir, and fermented foods, also play a role. By supporting healthy vaginal and gut flora, probiotics create an environment less favorable for harmful bacteria to thrive. This is especially valuable for women who take antibiotics frequently, as antibiotics can disrupt beneficial bacteria.
Other dietary strategies include reducing excessive sugar intake, since sugar can feed harmful bacteria, and including foods rich in vitamin C, which may help acidify urine and reduce bacterial growth.
Sexual Health and UTIs
Sexual activity is a well-known trigger for UTIs in women, sometimes referred to as “honeymoon cystitis.” During intercourse, bacteria can be pushed into the urethra, where they may cause infection. This does not mean women should avoid intimacy, but it does highlight the importance of preventive measures.
Urinating before and after sex, washing gently, and avoiding spermicides can reduce the risk. For women with recurrent UTIs linked to sex, healthcare providers may recommend post-coital antibiotics, which are taken only after intercourse to prevent infection.
Open conversations with partners also matter. Shame or silence around sexual health can prevent women from seeking the support they need. Recognizing UTIs as a medical condition—not a taboo topic—can empower women to protect their health without fear of judgment.
The Menopause Connection
Menopause brings profound changes to the female body, many of which increase susceptibility to UTIs. As estrogen levels decline, the protective lining of the vagina and urethra thins, and beneficial bacteria like Lactobacillus decrease. This shift creates an environment where harmful bacteria can flourish.
Hormone replacement therapies, particularly localized estrogen treatments, have been shown to restore some of this protective effect. Vaginal estrogen creams or rings can reduce recurrent UTIs in postmenopausal women without the risks associated with systemic hormone therapy.
Acknowledging this stage of life is essential. UTIs during menopause are not simply bad luck but a consequence of biological changes. Addressing them with compassion and evidence-based strategies helps women maintain quality of life.
Fast Relief When Symptoms Strike
When a UTI begins, the discomfort can escalate rapidly. The burning sensation, the urgency, and the constant trips to the bathroom make fast relief a priority. While antibiotics remain the gold standard for treating bacterial UTIs, there are steps women can take to ease discomfort while awaiting medical care.
Drinking large amounts of water helps dilute urine and flush bacteria. Applying a warm heating pad to the lower abdomen can relieve pain and cramping. Over-the-counter medications like phenazopyridine provide temporary relief of burning and urgency, though they do not treat the underlying infection.
It is crucial to seek medical attention promptly, especially if symptoms include fever, back pain, or nausea—signs that the infection may have reached the kidneys. Untreated UTIs can lead to serious complications. Fast relief is important, but proper treatment ensures full recovery.
Antibiotics: Benefits and Cautions
Antibiotics revolutionized the treatment of UTIs, transforming a once dangerous infection into a manageable condition. A short course—often three to seven days—can clear most infections effectively. For women with recurrent UTIs, doctors may prescribe longer courses or preventive regimens.
However, antibiotics are not without challenges. Overuse contributes to antibiotic resistance, a global health crisis. Resistant bacteria make infections harder to treat and limit available options. Antibiotics can also disrupt the natural balance of beneficial bacteria, sometimes leading to yeast infections or gastrointestinal upset.
Responsible use is key. Women should complete the prescribed course, even if symptoms improve quickly, and avoid self-medicating with leftover antibiotics. Doctors may also recommend urine cultures before prescribing, ensuring the chosen antibiotic targets the specific bacteria causing the infection.
Natural and Complementary Approaches
Beyond antibiotics, many women seek natural remedies to prevent or manage UTIs. While some lack strong scientific backing, others show promising results.
D-mannose, a natural sugar found in fruits like cranberries, has gained attention for its ability to prevent bacterial adhesion in the urinary tract. Studies suggest it may be as effective as low-dose antibiotics in preventing recurrent UTIs.
Herbal remedies such as uva ursi and garlic extracts have antimicrobial properties, though more research is needed. Adequate sleep, stress management, and a strong immune system also play crucial roles in preventing infections.
Natural approaches are not replacements for antibiotics when infections are established, but they can complement conventional care and reduce recurrence. Women should always discuss supplements with healthcare providers to ensure safety and avoid interactions.
The Challenge of Recurrent UTIs
For some women, UTIs are not an occasional inconvenience but a recurring nightmare. Recurrent UTIs—defined as three or more infections in a year or two within six months—affect millions worldwide. They require a more comprehensive approach to prevention and management.
Doctors may recommend low-dose daily antibiotics, post-coital antibiotics, or non-antibiotic options like D-mannose and vaginal estrogen. Lifestyle adjustments, from hydration to dietary changes, also play a role.
Equally important is emotional support. Recurrent UTIs can lead to feelings of helplessness, anxiety, and even depression. Women benefit from compassionate care that acknowledges not just the infection but the broader impact on quality of life.
When to Seek Immediate Medical Care
While most UTIs are uncomplicated, certain signs indicate a more serious infection that requires urgent attention. Fever, chills, flank or back pain, nausea, or vomiting suggest the infection may have spread to the kidneys. Left untreated, such infections can lead to sepsis, a life-threatening condition.
Pregnant women with UTIs also require prompt treatment, as infections can increase the risk of complications for both mother and baby.
Trusting your instincts matters. If symptoms feel severe, unusual, or rapidly worsening, medical care should not be delayed. Early intervention saves not only discomfort but potentially lives.
The Future of UTI Prevention
Science continues to explore new frontiers in UTI prevention and treatment. Vaccines targeting E. coli and other bacteria are in development, offering hope for long-term protection. Advances in microbiome research may lead to probiotic therapies that restore natural defenses more effectively.
Personalized medicine, guided by genetic and microbial profiling, could one day tailor prevention strategies to each woman’s unique biology. The future holds promise for fewer antibiotics, more targeted therapies, and a deeper understanding of the complex relationship between humans and microbes.
Living Free from Fear
A UTI can feel like a small infection with an outsized impact. It disrupts daily routines, clouds intimacy with worry, and leaves women wary of the next flare-up. Yet knowledge is power. By understanding how UTIs develop, how they can be prevented, and how to find fast relief, women can take back control of their health.
Prevention is not about perfection but about consistent habits: drinking water, practicing gentle hygiene, supporting the body with good nutrition, and seeking medical care when needed. Relief is about acting quickly, combining comfort measures with effective treatment.
Most importantly, living free from fear means recognizing that UTIs are not a reflection of weakness but a common human challenge—one that millions of women share. With science, compassion, and self-care, it is possible not only to overcome infections but also to thrive with confidence and resilience.