In a groundbreaking study published in JAMA Surgery, researchers from Harvard Medical School have revealed a startling and deeply unsettling finding: U.S. surgeons have a cancer mortality rate more than twice that of nonsurgeon physicians, and significantly higher than other professional and non-professional groups alike.
The investigation, led by some of the nation’s top medical minds, set out to understand how surgeons, who sit at the pinnacle of medical expertise and generally benefit from exceptional health knowledge, fare in terms of long-term mortality. The answer—especially regarding cancer—was anything but expected.
While surgeons still live longer on average than the general public, this study spotlights a previously undetected vulnerability in one of medicine’s most demanding professions. It raises new questions about how the high-intensity world of surgery might be quietly shaping long-term health risks, particularly those related to cancer.
The Numbers That Tell a Troubling Story
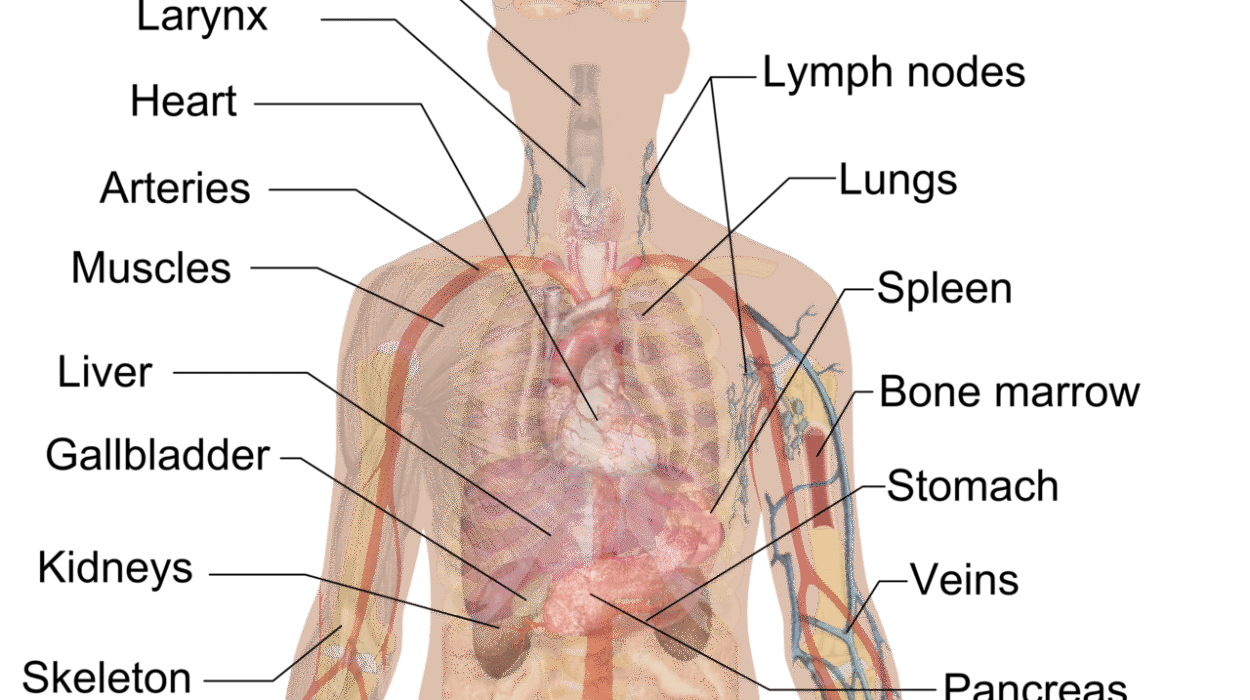
The Harvard-led team analyzed death data for over 1 million Americans aged 25–74 using 2023 data from the National Vital Statistics System. Among those studied were 224 surgeons and 2,740 nonsurgeon physicians, alongside large samples of professionals like engineers and lawyers, and the broader U.S. workforce.
Across the board, physicians had lower death rates than non-physician workers—a testament to their access to healthcare, healthy lifestyles, and overall education. But when surgeons were compared specifically to their nonsurgical counterparts, the story changed.
Surgeons recorded 355.3 deaths per 100,000 population, while nonsurgeon physicians had 228.4 deaths per 100,000, yielding a mortality rate ratio (MRR) of 1.56. This 56% higher death rate stunned researchers.
Even more revealing was the breakdown by cause of death. Cancer stood out starkly. While nonsurgeon physicians had a cancer mortality rate of 87.5 per 100,000, surgeons were dying of cancer at more than twice that rate: 193.2 per 100,000. That means cancer is the only major cause of death where surgeons not only fare worse than other physicians—but also worse than all other workers.
This is not a statistical fluke. The difference in cancer deaths is large enough to drive most of the overall mortality gap between surgeons and other physicians. If surgeons had cancer death rates equal to their nonsurgical peers, the mortality difference would nearly vanish.
Are the Operating Rooms Making Surgeons Sick?
So what’s happening? Why would surgeons, with their immense medical training and access to healthcare, face such elevated cancer risks?
The study doesn’t claim definitive answers—but it does strongly suggest that workplace exposure may be to blame.
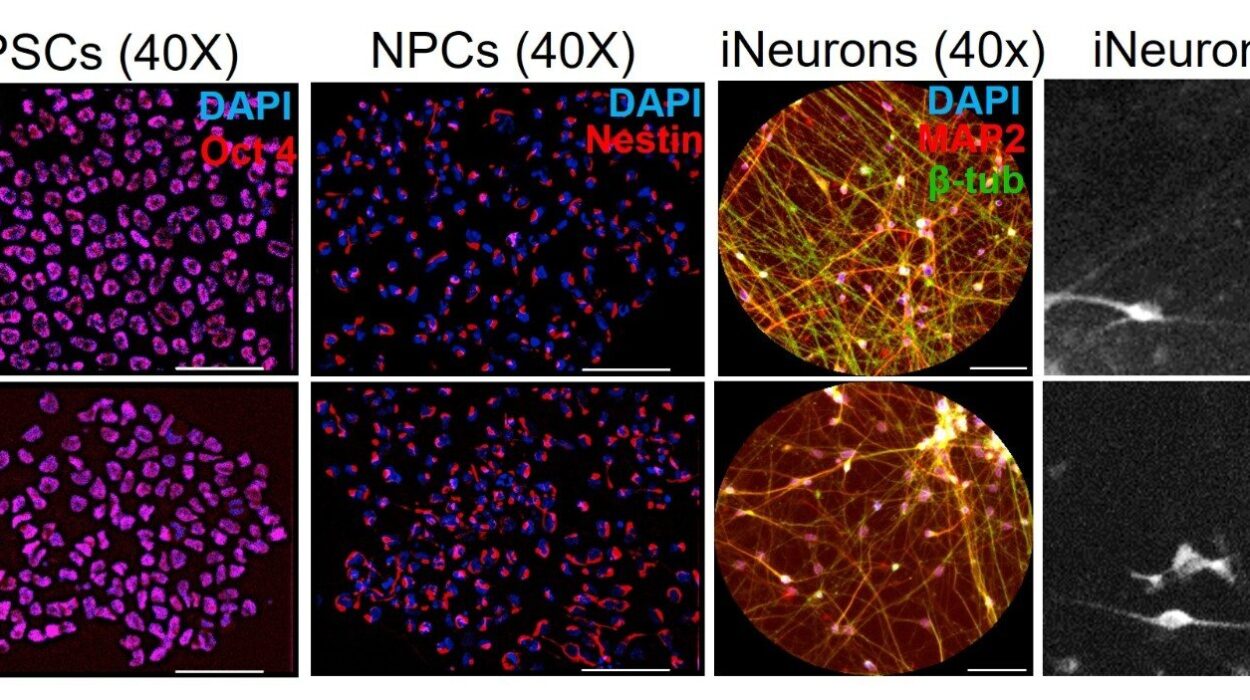
Operating rooms are environments filled with unique hazards. Surgeons spend hours in enclosed spaces under intense artificial lighting, often exposed to chemical sterilizers, anesthetic gases, radiation from imaging equipment, and even surgical smoke. This smoke, created when tissue is cauterized or cut using lasers or electrosurgical tools, has been shown to contain carcinogenic compounds, including benzene and formaldehyde.
Surgeons, particularly those in high-volume or high-complexity specialties, may spend thousands of hours in this environment over the course of a career. Even with modern ventilation systems and safety measures, long-term cumulative exposure could silently take its toll.
Additionally, stress and sleep deprivation are defining features of surgical life. Long hours, overnight shifts, and the intense pressure of high-stakes procedures can impair immune function and reduce the body’s ability to fight off early-stage cancers. Chronic stress has also been linked to increased risk of several cancers, including breast, colon, and prostate.
Surgeons are often expected to embody perfection under pressure—yet their profession may be grinding them down from the inside.
How the Rankings Reveal Hidden Dangers
In understanding why this cancer spike is so significant, it’s important to look at how cause-of-death rankings shift depending on occupational group. For example, car accidents are the fourth leading cause of death for surgeons, whereas for nonsurgeon physicians, they rank ninth. That doesn’t mean surgeons are reckless drivers—it reflects lower death rates in other categories (like respiratory diseases and diabetes) that push accidents higher on the list.
Surgeons are actually less likely than the average worker to die in a car accident (13.4 vs. 16.6 per 100,000), and far less likely to die from respiratory illness (0.6 vs. 27.0 per 100,000), diabetes, or influenza.
But cancer is different. While most causes of death are lower for surgeons compared to the general public, cancer is worse. It’s the only category where their mortality exceeds even non-physician workers, whose cancer death rate stands at 162 per 100,000.
This pattern is striking—and deeply concerning. It suggests that something specific to the surgical profession is responsible for the added risk.
What This Means for the Future of Medicine
These findings come at a time when the medical profession is already grappling with high rates of burnout, emotional distress, and early retirement. Now, with evidence of elevated cancer mortality among surgeons, the conversation must expand beyond mental health and work-life balance. The long-term physical health of surgeons is clearly at stake.
This study may serve as a wake-up call for hospital administrators, occupational health experts, and medical educators. If surgeons are suffering from hidden exposures, then current safety protocols—however well-intentioned—may not be sufficient.
More research is urgently needed. Longitudinal studies that track surgical professionals throughout their careers could help isolate risk factors. Additional investigations into specific exposures in the operating room—especially surgical smoke and ionizing radiation—are critical. And awareness campaigns could help physicians themselves better understand the hidden dangers of their work environments.
The medical community owes it not only to its surgeons, but also to the countless lives they save, to ensure that their own lives are not quietly shortened by the very profession they’ve devoted themselves to.
The Paradox of Knowledge and Vulnerability
Perhaps the most poignant aspect of this study is its quiet paradox: that those who save lives for a living may be sacrificing their own health in the process—not through heroic selflessness, but through routine, invisible hazards that accrue over time.
It challenges the assumption that knowledge is always power. The surgeons in this study are not ignorant of cancer risk. They are, in many ways, the best informed. But when the danger comes from the very tools and spaces required to do their jobs, even the deepest knowledge may not offer protection without institutional change.
This new research doesn’t aim to panic the public—or surgeons. Rather, it opens a door to understanding and action. It reminds us that every profession carries hidden costs, and that science, even when unsettling, offers the best path to solving problems that live in the shadows.
As we applaud the steady hands of surgeons in the operating theater, we must also ask: who is caring for them?
Because now, more than ever, it’s clear—they need our care, too.
More information: Vishal R. Patel et al, Mortality Among Surgeons in the United States, JAMA Surgery (2025). DOI: 10.1001/jamasurg.2025.2482