For decades, doctors have struggled to explain one of the most common yet least understood forms of heart failure: heart failure with preserved ejection fraction (HFpEF). Affecting nearly 4 million people in the United States and 32 million worldwide, HFpEF is a condition where the heart remains strong enough to pump, but too stiff to relax and fill properly. Patients often feel breathless with even mild exertion, and fluid can build up in the lungs, legs, or abdomen. Despite its prevalence, HFpEF has long baffled the medical world.
Now, a new paper published in the Journal of the American College of Cardiology (JACC) and presented at the ESC Congress 2025 proposes a groundbreaking way of understanding this condition. Authored by Milton Packer, MD, FACC, Distinguished Scholar in Cardiovascular Science at Baylor University Medical Center and Visiting Professor at Imperial College London, the study introduces what is being called the Adipokine Hypothesis.
This new framework offers not only an explanation of how HFpEF develops, but also a roadmap toward more effective treatments.
The Role of Internal Fat in Heart Failure
Traditionally, HFpEF was thought to be primarily linked to high blood pressure. But that explanation fell short—many patients with HFpEF did not fit neatly into the “hypertension leads to heart failure” story. Instead, nearly all patients shared another trait: an excess of internal fat tissue, especially around vital organs like the heart.
Until now, the mechanism connecting this internal fat to heart dysfunction was poorly understood. Dr. Packer’s Adipokine Hypothesis changes that.
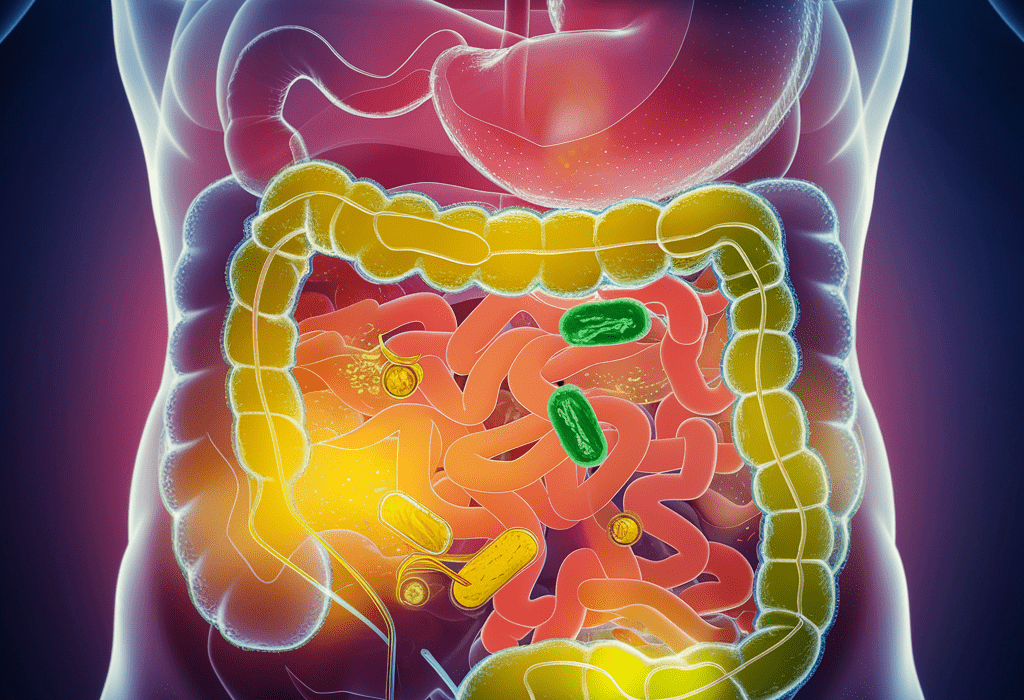
Fat tissue is not inert. It is biologically active, releasing signaling proteins called adipokines that allow fat to communicate with the rest of the body. In healthy amounts, adipokines protect the heart and kidneys by reducing stress, calming inflammation, and maintaining fluid balance. But when there is too much internal fat, the biology of this tissue changes. Instead of sending protective signals, the fat releases harmful adipokines that promote stress, inflammation, and scarring inside the heart.
This transformation, according to the Adipokine Hypothesis, is the missing link that drives HFpEF.
Shifting the Focus of Treatment
Perhaps the most powerful implication of the hypothesis is its impact on treatment. For years, therapies for HFpEF focused directly on the heart, with limited success. But if the root cause lies in fat tissue, then targeting that tissue may be the key.
Experimental studies support this idea: drugs that alter fat tissue’s adipokine profile can improve HFpEF symptoms, not by acting on the heart itself, but by restoring the healthy balance of signaling molecules.
Some of these treatments already exist. Drugs that shrink or change fat tissue—including GLP-1 receptor agonists like semaglutide and tirzepatide—can favorably shift adipokine release. These medications, originally developed for diabetes and now widely used for weight management, may also represent a powerful tool against HFpEF.
“The Adipokine Hypothesis points us toward drugs that already have FDA approval,” Packer explained. “The challenge is that they are not being widely prescribed for HFpEF—yet.”
Moving Beyond BMI: Waist-to-Height Ratio
Another critical insight from the paper is the need to rethink how doctors identify patients at risk. Traditionally, obesity has been defined by body mass index (BMI), a simple calculation of weight divided by height. But BMI has serious limitations—it doesn’t distinguish between muscle, bone, and fat, nor does it reveal where fat is stored in the body.
Instead, Packer emphasizes the importance of the waist-to-height ratio as a more accurate marker of excess internal fat.
- A healthy ratio is less than 0.5 (waist smaller than half of height).
- Patients with HFpEF usually have a ratio greater than 0.5, often over 0.6.
This measure can reveal dangerous fat deposits even when BMI appears normal. “In patients with an elevated waist-to-height ratio, clinicians should be very vigilant,” Packer said. “Many people who are short of breath assume obesity is to blame, when in fact, the true cause may be HFpEF—which is treatable.”
Echoes of a Past Breakthrough
For Dr. Packer, this is not the first time he has proposed a unifying theory for heart failure. Thirty-three years ago, he introduced the neurohormonal hypothesis for heart failure with reduced ejection fraction (HFrEF). That landmark paper transformed how doctors approached treatment, leading to therapies that have saved millions of lives.
The new Adipokine Hypothesis could play a similar role for HFpEF, offering clarity where confusion has long reigned.
A Future of New Hope
The implications of this hypothesis stretch far beyond the walls of cardiology clinics. They reshape how we think about fat, metabolism, and heart disease itself. Fat is not simply a matter of appearance or weight—it is a powerful biological force, capable of either protecting or damaging the heart depending on its balance.
With new tools to measure risk, and new therapies that restore the healthy biology of fat tissue, patients with HFpEF may finally see more effective treatments. And for millions who struggle with breathlessness, swelling, and fatigue, that means not only better health, but renewed hope.
Science is at its best when it unravels mysteries and points us toward healing. The Adipokine Hypothesis does just that, reframing our understanding of HFpEF and opening the door to a future where this silent, stubborn form of heart failure can be tackled at its true source.