In a world racing to understand and halt the advance of neurodegenerative diseases, a groundbreaking study led by Professor Kiavash Movahedi of the Brussels Center for Immunology at the Vrije Universiteit Brussel is lighting the path forward. Published in the prestigious journal Immunity, this international collaboration is not just another brick in the scientific wall—it could be the keystone for a revolutionary therapy against debilitating disorders like Alzheimer’s and Parkinson’s disease.
This discovery pierces the veil of what was long considered an impenetrable barrier: the challenge of replacing microglia, the brain’s elusive immune cells. Long thought irreplaceable, these ancient guardians of the central nervous system may now have suitable stand-ins—heralding a new chapter in neuroimmunology and regenerative medicine.
The Mysterious Microglia: Sentinels of the Central Nervous System
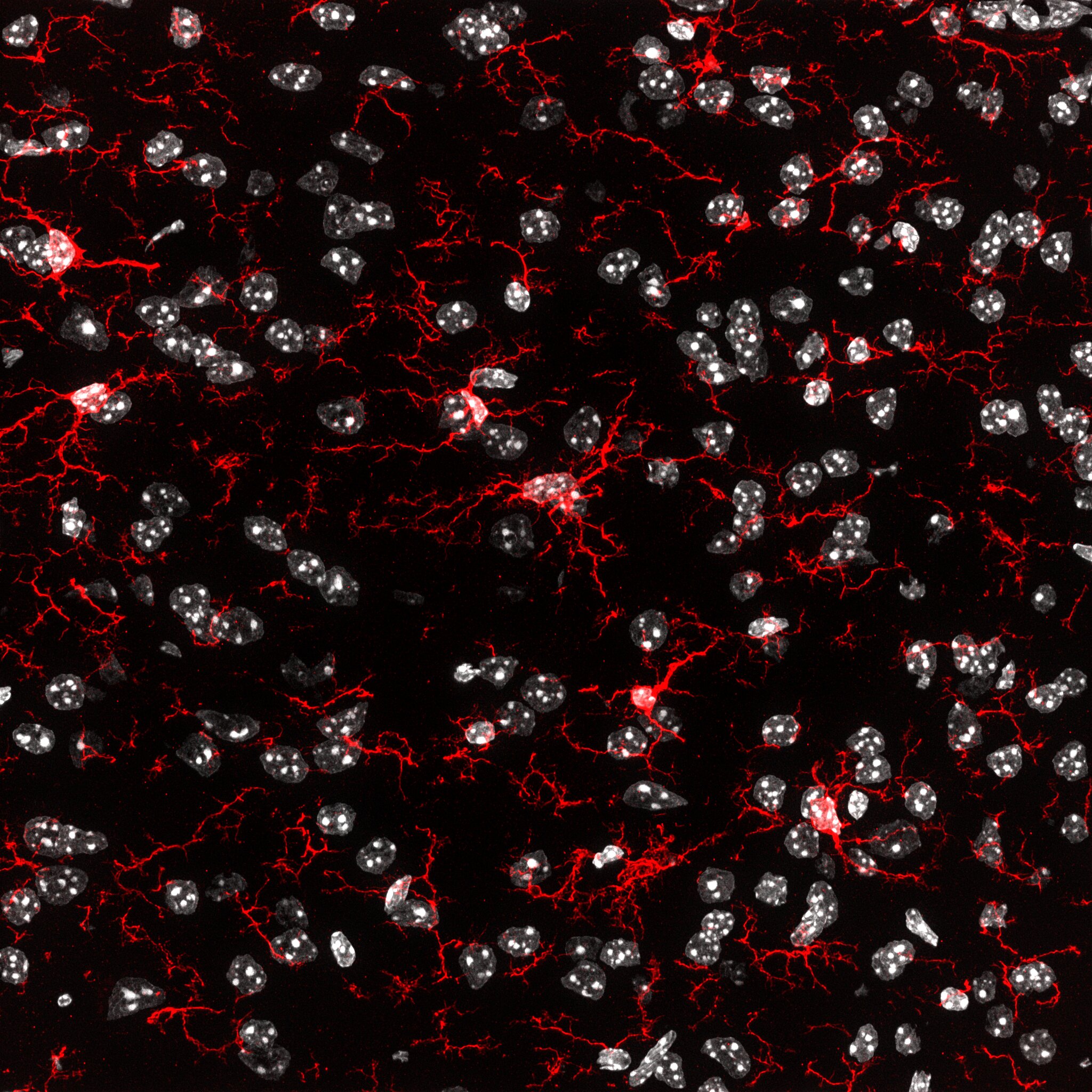
To understand the magnitude of this discovery, one must first grasp the enigmatic nature of microglia. Often described as the brain’s immune sentinels, microglia are more than mere scavengers of cellular debris. They prune synapses during development, monitor neuronal health, and respond swiftly to signs of infection, injury, or dysfunction.
“Microglia are unique,” explains Prof. Movahedi. “They originate early in embryonic development and maintain themselves throughout life without being replaced by new cells from the blood. That makes them special, but also vulnerable.”
Unlike other immune cells, microglia don’t regenerate from the bone marrow. They form from primitive yolk sac progenitors before birth and persist through self-renewal. This exclusivity confers remarkable specialization, but also a dangerous rigidity. Once damaged, microglia cannot easily be replaced or repaired—and this rigidity is now believed to play a major role in the progression of neurodegenerative diseases.
The Challenge: Can the Brain Accept Outsiders?
Attempts to replace microglia have previously hit a dead end. The blood-brain barrier—a formidable shield that restricts the entry of cells and molecules—prevents foreign immune cells from infiltrating the brain under normal conditions. This isolation, while essential for protecting the brain from infection and inflammation, poses a dilemma for cell-based therapies.
Moreover, even if new cells manage to sneak in, convincing them to behave like native microglia is another Herculean task. The brain’s microenvironment is extraordinarily complex, and only a narrow subset of cells can adapt to it.
But that may be changing.
A New Hope: Monocytes as Microglial Replacements
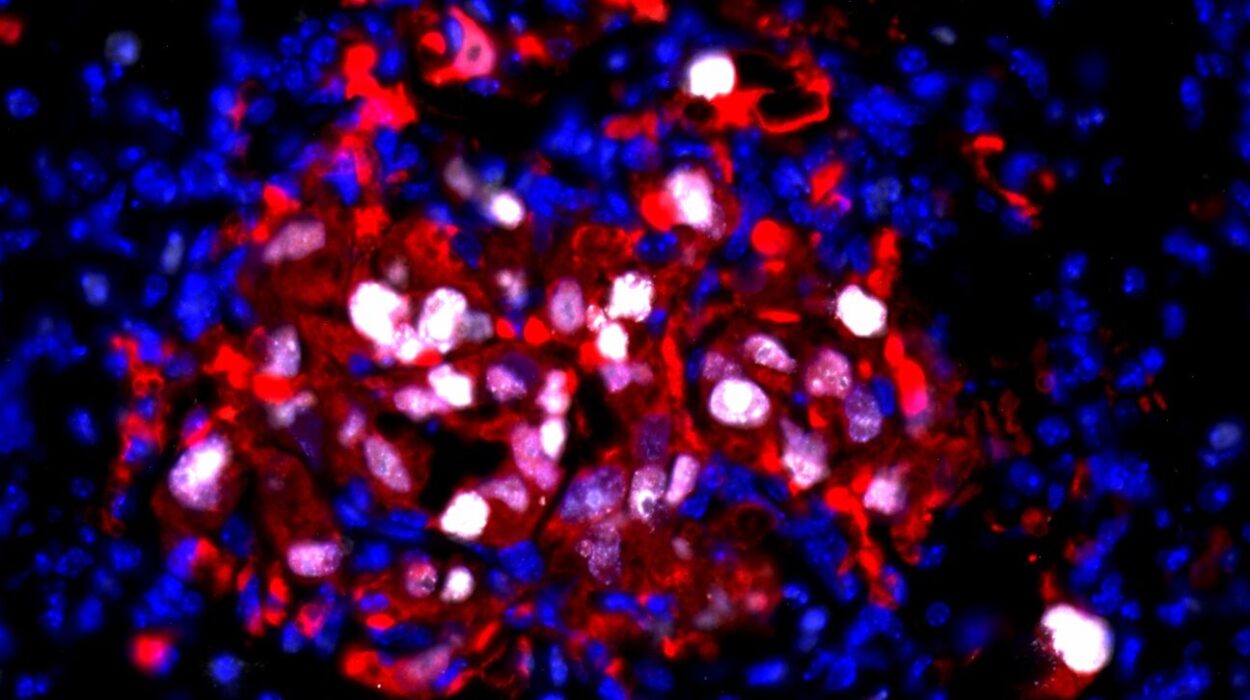
In their new study, Movahedi’s team demonstrated for the first time that under carefully engineered conditions, white blood cells known as monocytes can be coaxed across the blood-brain barrier to settle and function within the brain’s intricate ecosystem.
“This opens up new avenues for future therapies,” Movahedi says, with a hint of both optimism and caution.
Monocytes, which normally circulate in the bloodstream as part of the body’s immune defense, are a more accessible and renewable resource compared to microglia. By manipulating signaling pathways and the brain’s cellular landscape, the researchers were able to “invite” these monocytes into the brain and watch them adopt roles similar to those of microglia.
But it wasn’t a perfect transformation.
The Identity Dilemma: Close Imitators, Yet Molecularly Distinct
“Although they mimic microglial functions, they remain molecularly distinct,” notes Jonathan Bastos, Ph.D. researcher and first author of the study. “This may be a disadvantage, as the new cells may not be able to fully replicate the normal functions of microglia.”
Indeed, while the transplanted monocytes could respond to injury and inflammation in ways reminiscent of microglia, they carried a different molecular signature. This distinction matters. Microglia are not just general immune cells—they are sculpted by their embryonic origins and the brain’s developmental environment to carry out incredibly nuanced tasks.
Therefore, even a near-perfect imitation might fall short in long-term safety or effectiveness. The question becomes: can we do better?
Back to the Beginning: The Power of Embryonic Origins
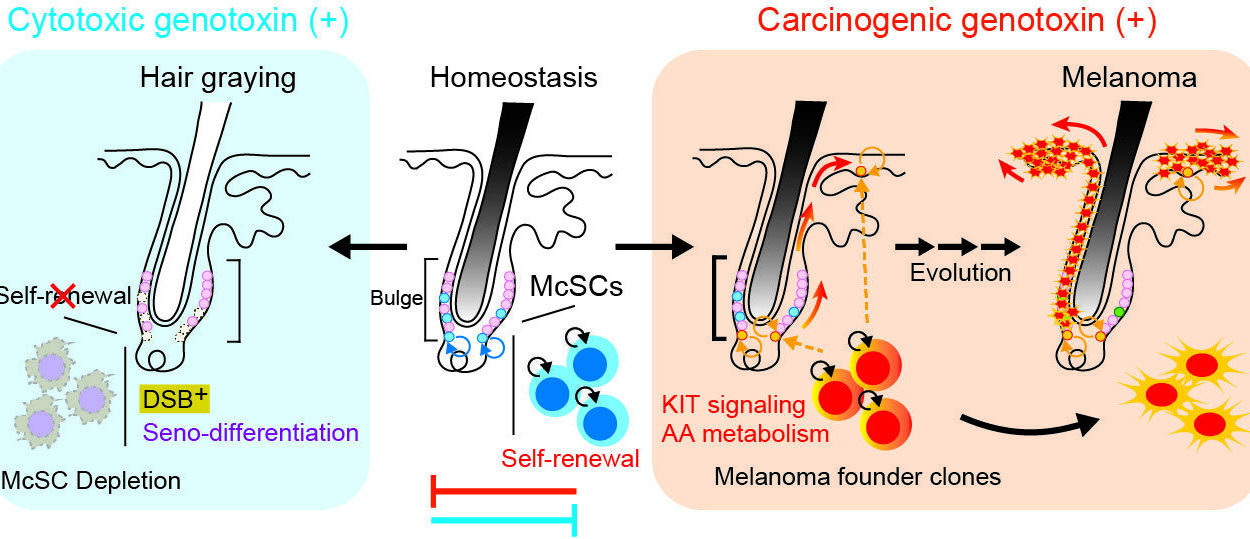
One of the most exciting discoveries in the study came from tracing the developmental lineage of microglia. The team found that monocytes derived from embryonic precursors—rather than adult immune cells—were far more adept at adopting a true microglial identity.
This echoes what nature has already shown us. Microglia originate from the yolk sac during the first few weeks of embryogenesis and are distinct from bone marrow-derived monocytes. Their unique gene expression profiles, shaped in the womb, allow them to develop and maintain the central nervous system’s delicate balance over a lifetime.
By leveraging embryonic stem cells or reprogramming adult cells into microglia-like cells with yolk sac characteristics, scientists could recreate a more authentic microglial population for transplantation.
This isn’t just a scientific novelty—it could be the blueprint for a new class of brain-specific cell therapies.
From Bench to Bedside: Toward Personalized Cell Therapy
Building on these findings, the team is now working to develop strategies for personalized medicine. The goal: use a patient’s own cells, reprogrammed and refined, to replace damaged microglia with functionally equivalent or even enhanced versions.
This approach, while still experimental, could eliminate the risk of immune rejection and ensure long-term integration into the brain’s tissue. Furthermore, researchers are exploring the possibility of engineering these new microglia to produce therapeutic substances—such as neuroprotective proteins or anti-inflammatory agents—directly within the brain.
Imagine a future where not only can we replace the faulty cells that contribute to neurodegenerative disease, but also arm those replacements with molecular tools to actively fight disease progression. It would be akin to turning microglia into intelligent repair agents—cellular “trojan horses” trained to heal rather than harm.
The Power of Collaboration: An International Effort
The breakthrough was not achieved in isolation. Movahedi’s group collaborated with international partners across Europe and North America, combining insights from immunology, neurobiology, and stem cell research.
Of particular importance was a simultaneous study by American researchers, led by F. Chris Bennett, which provided compelling in vivo data. Using a mouse model, the U.S. team demonstrated that the replacement therapy not only established new microglia-like cells in the brain but also resulted in measurable improvements in neurological function.
This convergence of basic science and applied research strengthens the case for future clinical applications.
“The work of colleague F. Chris Bennett provides evidence that this new approach truly holds potential,” Movahedi emphasizes.
A Timely Discovery in the Face of a Global Crisis
Neurodegenerative diseases are among the most pressing medical challenges of our time. According to the World Health Organization, Alzheimer’s and other forms of dementia affect more than 55 million people worldwide—a number expected to double by 2050. Parkinson’s disease, meanwhile, continues to rise sharply in prevalence, with millions affected globally.
Current treatments offer only symptomatic relief, with no cure in sight. Worse, many drugs fail to halt or even meaningfully slow disease progression.
This new microglia replacement strategy could fundamentally alter that landscape. Rather than patching symptoms, it aims to restore the brain’s natural defense and maintenance system. And with future iterations incorporating gene editing or therapeutic protein production, the possibilities for durable, disease-modifying treatments expand dramatically.
Looking Ahead: The Beginning of a New Era
Science is often a tale of incremental gains, but occasionally, it leaps. The discovery that microglia—long considered irreplaceable—can be functionally and therapeutically replaced is one such leap.
Of course, much work remains. Researchers must refine protocols, ensure long-term safety, and validate results in human trials. The ethical and regulatory landscape for cell-based brain therapies also presents challenges. But the momentum is undeniable.
“We are still at the beginning,” says Movahedi. “But our results lay a foundation on which to build innovative treatments that not only alleviate symptoms but actually tackle the root causes.”
This is more than just a scientific breakthrough; it’s a testament to human ingenuity, collaboration, and the relentless pursuit of healing. For millions suffering from the slow erosion of memory, movement, and identity, it offers something even more precious than knowledge—hope.
Reference: Monocytes can efficiently replace all brain macrophages and fetal liver monocytes can generate bona fide Sall1+ microglia., Immunity (2025). DOI: 10.1016/j.immuni.2025.04.006. www.cell.com/immunity/fulltext … 1074-7613(25)00169-4