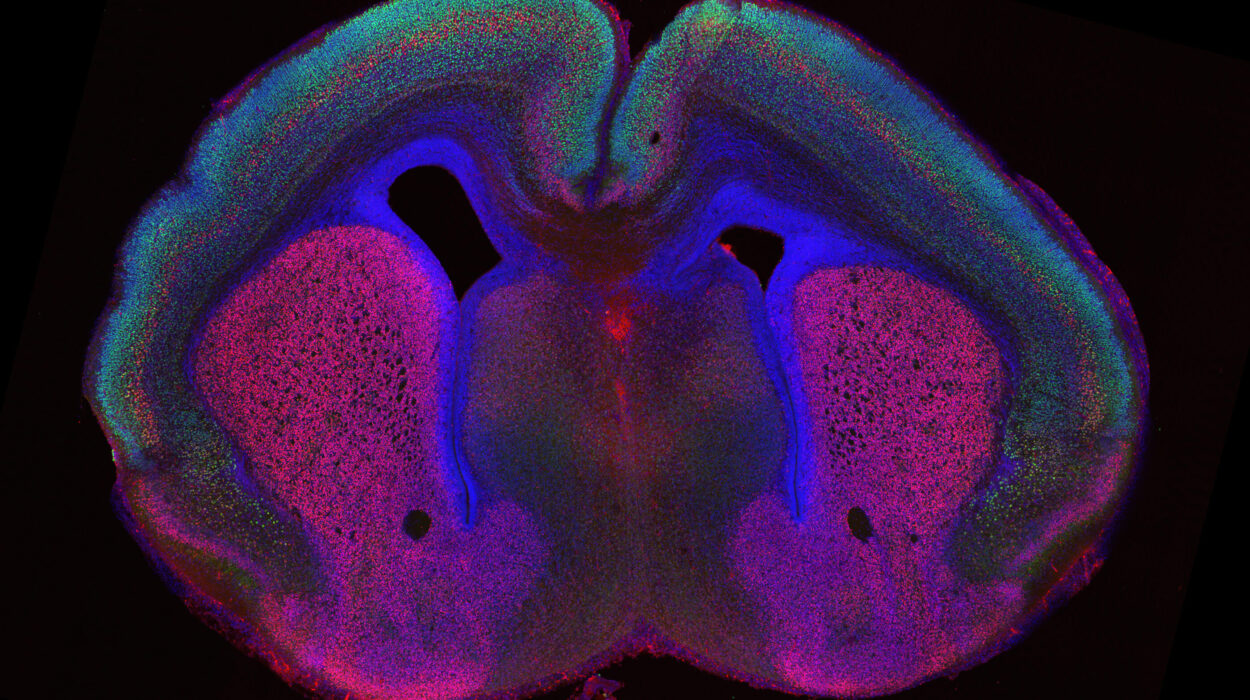
The relentless nature of glioblastoma, one of the most aggressive forms of brain cancer, has long left doctors with few options for patients. This devastating disease, which forms from the brain’s astrocytes, progresses rapidly and often leads to a grim diagnosis. Despite advances in cancer treatment, glioblastoma remains nearly impossible to treat effectively, partly because delivering drugs to the brain is a complex and invasive process. But a team of researchers at Washington University in St. Louis, in collaboration with Northwestern University, has just turned this challenge on its head, offering a glimmer of hope for patients with this deadly condition.
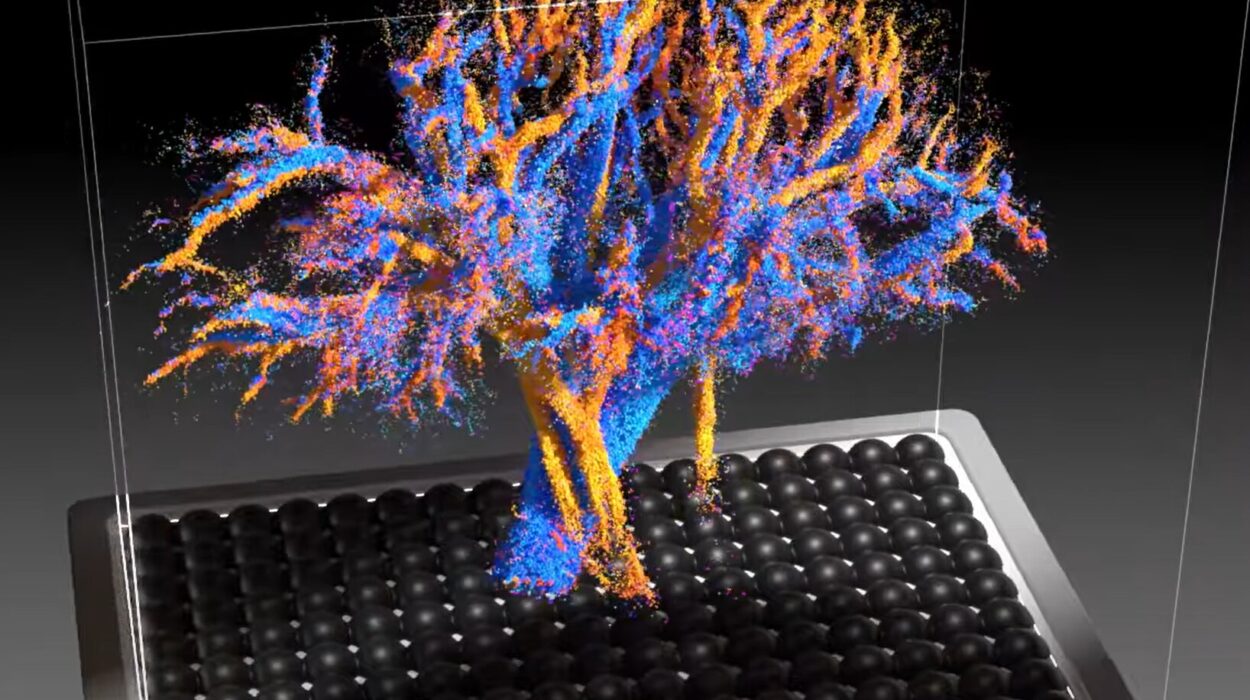
Their breakthrough lies in an innovative, noninvasive approach that uses nasal drops to deliver potent cancer-fighting drugs directly to the brain. This new method relies on tiny, precisely engineered nanoparticles to activate the brain’s immune system, enabling it to better attack and fight glioblastoma. The results, published in the journal PNAS, show promise in mouse models, opening the door to a future where glioblastoma and other immune-resistant cancers might finally be defeated.
Nanotechnology Meets the Nose
For years, researchers have tried to find ways to deliver treatments to the brain without resorting to the highly invasive methods currently in use, such as direct tumor injections. This new study presents an elegant solution that bypasses these methods entirely. Instead, researchers turned to a part of the body that is often overlooked in drug delivery: the nose.
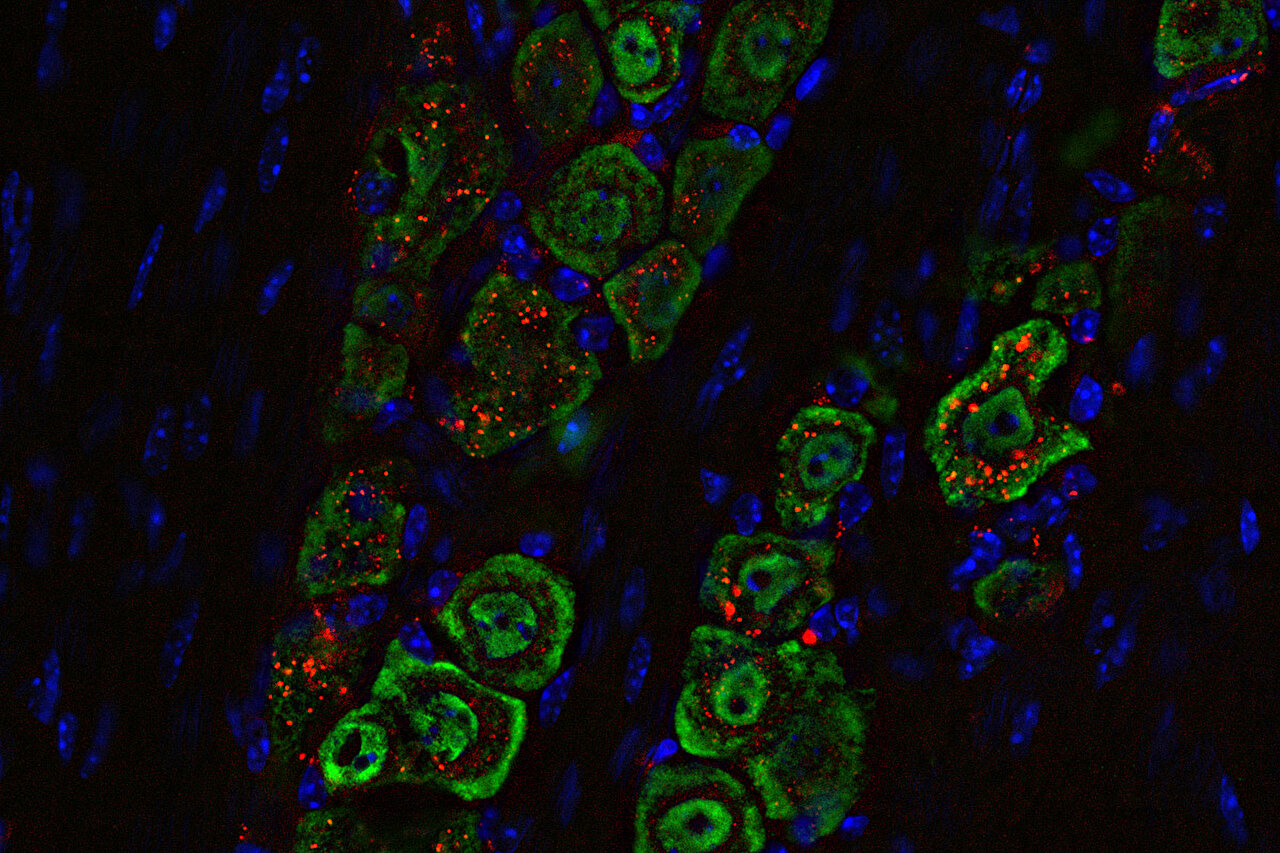
The idea of delivering drugs through the nasal passages to treat brain diseases isn’t new, but it has never been successfully applied at the nanoscale, especially for activating immune responses against cancers like glioblastoma. This time, however, the team led by Alexander Stegh, Ph.D., at Washington University’s School of Medicine, found a way to use the nasal route to deliver nano-sized therapeutic structures called spherical nucleic acids. These nanoparticles are engineered to carry DNA or RNA that activates the immune system, and they’ve shown greater therapeutic potential than other delivery methods.
“We wanted to change this reality and develop a noninvasive treatment that activates the immune response to attack glioblastoma,” Stegh explained. The goal was to create a treatment that was not only effective but also less invasive and more patient-friendly. The team succeeded in using the power of nanotechnology to create a new approach to brain cancer treatment—one that doesn’t require cutting into the skull or injecting drugs directly into the tumor.
The STING Pathway and Cold Tumors
Glioblastomas are notoriously difficult to treat because they are “cold tumors,” meaning they don’t trigger a strong immune response in the body. This makes it hard for the body’s natural defenses to target and destroy the cancer cells. In contrast, “hot tumors” are more easily targeted by immune therapies because they already provoke an immune reaction.
In the case of glioblastoma, researchers have been exploring ways to activate the immune system to recognize and fight the tumor. One promising strategy involves the STING pathway, which is triggered when cells detect foreign DNA, activating the immune system to launch an attack. The team’s new nanotechnology approach aimed to use spherical nucleic acids to activate this pathway in glioblastoma cells, a move that has shown potential in earlier studies. The challenge, however, has always been delivering the therapeutic agents to the brain in a way that avoids the need for invasive procedures.
“We really wanted to minimize patients having to go through that when they are already ill,” said Akanksha Mahajan, Ph.D., the study’s first author and a postdoctoral researcher in Stegh’s lab. Together with the help of Northwestern’s Chad A. Mirkin, Ph.D., the team used spherical nucleic acids to deliver STING-activating agents in a way that bypassed the need for direct injection into the tumor.
Nasal Drops Targeting the Brain
To test their approach, the researchers used a molecular tag visible under near-infrared light to track the nanoparticles. They discovered that when delivered as nasal drops into the mice’s noses, the nanoparticles traveled along the nerve that connects the face to the brain. Once inside, they activated immune responses, specifically targeting the tumor itself and the immune cells that surround it. This highly targeted delivery ensured that the medicine reached the brain without affecting other parts of the body, minimizing the risk of unwanted side effects.
The therapy proved to be effective. When combined with other immune-boosting treatments, the therapy not only activated the immune system to attack the tumor, but it also completely eradicated the glioblastoma in the mice with just one or two doses. The team’s method led to long-term immunity, preventing the tumors from returning. The results far exceeded what has been achieved with traditional STING-activating therapies.
A Step Toward Clinical Application
Though the results in mice were promising, Stegh cautioned that firing up the STING pathway alone isn’t enough to fully eradicate glioblastoma. The tumor itself has ways of blocking the immune system, which is why the researchers are now working to combine their approach with other immune-boosting strategies. By adding more capabilities to their nanoparticle platform, they hope to target multiple immune responses at once, increasing the therapy’s chances of success.
“This is an approach that offers hope for safer, more effective treatments for glioblastoma and potentially other immune treatment-resistant cancers, and it marks a critical step toward clinical application,” said Stegh.
The team’s work is still in its early stages, and much remains to be done before this treatment can be used in humans. But the breakthrough represents a significant step forward in the fight against glioblastoma and could eventually lead to noninvasive treatments for other cancers that evade the immune system. If successful, this technology could offer patients a safer, more effective way to battle one of the most deadly cancers known to humankind.
Why This Research Matters
This study is more than just a technical breakthrough; it’s a story of hope. Glioblastoma has long been a relentless adversary, with few treatment options and an overwhelmingly poor prognosis. For patients and their families, this new approach offers a glimmer of light in a dark tunnel. By using the body’s own immune system to fight cancer, and by delivering the treatment in a way that avoids invasive surgeries, researchers have paved the way for safer, more accessible therapies.
What’s even more exciting is the potential broader impact of this research. While glioblastoma is the immediate target, the same technology could one day be used to fight other cancers that are resistant to immune therapies. The team’s work also shines a light on the promise of nanotechnology in medicine—showing how tiny, precisely engineered materials can unlock new possibilities for treating diseases that were once thought untreatable.
As the study moves forward, the hope is that what begins in a lab with mice could one day be transformed into a life-saving treatment for humans. For now, the researchers are optimistic but aware of the challenges ahead. Still, they have proven one thing: in the fight against brain cancer, science may just have found a new, noninvasive weapon.
More information: Akanksha S. Mahajan et al, cGAS-agonistic spherical nucleic acids reprogram the glioblastoma immune microenvironment and promote antitumor immunity, Proceedings of the National Academy of Sciences (2025). DOI: 10.1073/pnas.2409557122