Trauma leaves marks. Sometimes those marks are visible—scars on the skin, broken bones, a body that carries the memory of violence or disaster. But sometimes, trauma hides deep within the mind, where it continues to echo long after the danger has passed. This is the world of Post-Traumatic Stress Disorder, or PTSD, a condition that affects millions worldwide.
For someone with PTSD, a loud sound may feel like gunfire, a crowded street may feel like a battlefield, and sleep may become haunted by recurring nightmares. While time heals many wounds, PTSD shows us that the mind does not always move on just because life around us does. The memories linger, replaying themselves in painful loops that disrupt daily life, relationships, and a person’s very sense of self.
Understanding PTSD is not just about studying a medical diagnosis. It is about empathy for those who live with invisible injuries, recognition of the immense resilience of survivors, and a commitment to offering pathways of healing. In this article, we will explore what PTSD is, why it develops, how it manifests, and what can be done to help those who struggle with it.
What Is PTSD?
Post-Traumatic Stress Disorder is a psychiatric condition that develops after exposure to a traumatic event. Trauma, in this context, refers to experiences that overwhelm a person’s ability to cope, shattering their sense of safety and control. This might include combat, natural disasters, sexual assault, serious accidents, or witnessing violence.
While not everyone exposed to trauma develops PTSD, for some, the experience lodges so deeply in memory and emotion that it disrupts normal functioning long after the event has ended. The mind becomes stuck in survival mode, unable to distinguish between past danger and present safety.
PTSD is officially recognized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), where it is classified as a trauma- and stressor-related disorder. It is not a sign of weakness, but a response to extreme experiences that overwhelm normal adaptive mechanisms.
Causes of PTSD: Why Trauma Sticks
Not every traumatic experience leads to PTSD. Some individuals recover naturally, while others develop lingering symptoms. The reasons are complex, involving a blend of biology, psychology, and social context.
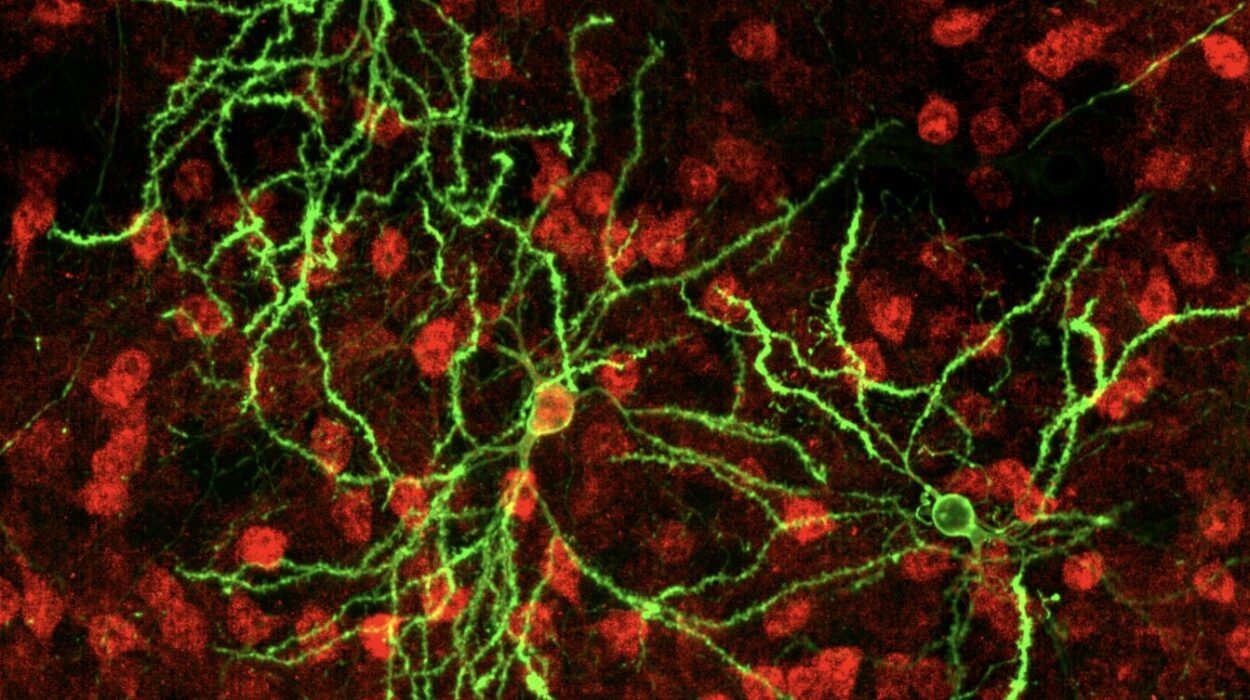
The Role of the Brain
Trauma fundamentally alters how the brain processes memory and threat. The amygdala, the brain’s alarm center, becomes hyperactive, constantly scanning for danger. Meanwhile, the hippocampus, which helps place experiences into context and time, may function abnormally, leading to fragmented, intrusive memories. The prefrontal cortex—the rational part of the brain that calms fear responses—may lose its regulatory grip.
Together, these changes mean that traumatic memories do not fade into the past. Instead, they remain vivid, raw, and easily triggered, making the survivor feel as though the danger is happening all over again.
Genetic and Biological Factors
Research shows that certain individuals may be biologically predisposed to developing PTSD. Variations in genes related to the stress response, neurotransmitters like serotonin, or the regulation of cortisol (the body’s stress hormone) can increase vulnerability. Additionally, previous trauma, particularly in childhood, can prime the nervous system to respond more intensely to later traumatic experiences.
Psychological and Social Factors
A person’s mental and emotional resilience also plays a role. Those with strong coping strategies, supportive relationships, and a sense of meaning may recover more effectively. On the other hand, lack of social support, prior mental health challenges, or ongoing stressors such as poverty and discrimination increase the risk of PTSD.
In essence, PTSD develops not just from what happened, but from how the brain, body, and environment respond to what happened.
Symptoms of PTSD: When the Past Refuses to Stay in the Past
PTSD is marked by a constellation of symptoms that can disrupt nearly every aspect of life. These symptoms often cluster into four main categories, though individuals may experience them differently.
Intrusive Memories
Trauma has a way of resurfacing, often at the most unexpected times. People with PTSD may experience:
- Recurrent, involuntary, and distressing memories of the traumatic event.
- Nightmares that replay the trauma or carry similar themes of danger and helplessness.
- Flashbacks, in which the person feels as though the event is happening again in real time.
These symptoms can be so vivid that the distinction between memory and reality blurs. A car backfiring may transport a combat veteran back to the battlefield; the smell of alcohol may throw a survivor into the terror of past abuse.
Avoidance
Because reminders of trauma trigger intense distress, many people with PTSD begin avoiding them. This may include avoiding certain places, people, conversations, or even thoughts and feelings. While avoidance may bring temporary relief, it often worsens symptoms in the long term by preventing emotional processing.
Negative Changes in Thinking and Mood
Trauma reshapes how people view themselves, others, and the world. Common symptoms include:
- Persistent negative beliefs (“I am broken,” “The world is dangerous,” “I cannot trust anyone”).
- Distorted blame directed at oneself or others.
- Persistent fear, guilt, or shame.
- Emotional numbness or detachment from others.
- Loss of interest in activities once enjoyed.
These changes can erode self-worth and relationships, leaving survivors isolated and disconnected.
Changes in Arousal and Reactivity
PTSD keeps the body’s alarm system on high alert. Symptoms may include:
- Hypervigilance—constantly scanning the environment for threats.
- Exaggerated startle response—jumping at sudden noises or movements.
- Irritability or angry outbursts.
- Difficulty concentrating.
- Sleep disturbances, including insomnia.
Living in a body that never feels safe takes a heavy toll, both physically and emotionally.
How PTSD Is Diagnosed
Diagnosing PTSD requires a careful, compassionate process. Mental health professionals use structured interviews, self-report questionnaires, and clinical observation to determine whether someone meets diagnostic criteria.
According to the DSM-5, a PTSD diagnosis requires exposure to a traumatic event and the presence of symptoms from each of the four clusters (intrusion, avoidance, negative alterations in cognition/mood, and arousal/reactivity) lasting more than one month. The symptoms must also cause significant distress or impairment in daily functioning.
It is important to distinguish PTSD from other conditions that may share similar features, such as depression, generalized anxiety, or substance use disorders. Many individuals with PTSD also experience these comorbid conditions, which can complicate diagnosis and treatment.
Treatment of PTSD: Pathways to Healing
The good news is that PTSD is treatable. While recovery is not always linear and symptoms may persist for years, many people experience significant improvement with the right interventions. Treatment approaches often combine psychotherapy, medication, lifestyle changes, and social support.
Psychotherapy: Healing Through the Mind
Therapy is the cornerstone of PTSD treatment. Evidence-based approaches include:
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and reframe distorted thoughts related to the trauma. A specialized form called Cognitive Processing Therapy (CPT) is particularly effective for PTSD.
- Prolonged Exposure Therapy (PE): Involves safely confronting traumatic memories and avoided situations, helping the brain process and integrate them rather than suppress them.
- Eye Movement Desensitization and Reprocessing (EMDR): Uses guided eye movements or other bilateral stimulation to help reprocess traumatic memories, reducing their emotional intensity.
- Trauma-Focused Therapy: Integrates elements of multiple therapeutic approaches to directly address the impact of trauma.
Therapy not only reduces symptoms but also helps individuals rebuild trust, meaning, and self-compassion.
Medications: Balancing the Brain’s Chemistry
Medications can be valuable in managing PTSD, particularly when symptoms are severe. Selective serotonin reuptake inhibitors (SSRIs) such as sertraline and paroxetine are commonly prescribed and have been approved by the FDA for PTSD treatment. Other medications may help with specific symptoms like nightmares or insomnia.
Medication is not a cure on its own but can provide relief that enables individuals to engage more effectively in therapy.
Lifestyle and Self-Care
Healing from PTSD is not only about clinical interventions but also about nurturing the body and mind in daily life. Exercise, mindfulness, yoga, and relaxation techniques have been shown to reduce stress and improve mood. Adequate sleep, balanced nutrition, and limiting substances like alcohol also play an important role.
Social connection is another critical factor. Supportive friends, family, and peer groups provide both understanding and encouragement, breaking the isolation that trauma often creates.
Emerging and Complementary Approaches
Research is exploring new frontiers in PTSD treatment, including psychedelic-assisted therapy (using substances like MDMA under controlled conditions), virtual reality exposure therapy, and neurofeedback. While still under study, these approaches hold promise for individuals who do not respond to traditional treatments.
Living With PTSD: Stories of Strength
While PTSD is often described in terms of symptoms and impairments, it is also a story of resilience. Many people with PTSD go on to rebuild fulfilling lives, finding meaning in their struggles and even using their experiences to help others. This concept, known as post-traumatic growth, highlights that suffering and growth can coexist.
For example, a veteran who endured combat trauma may later become an advocate for mental health awareness. A survivor of assault may find healing in supporting others through crisis hotlines or counseling. These stories remind us that PTSD does not define a person’s worth or future—it is a chapter in a larger narrative of human resilience.
Conclusion: Toward Compassion and Recovery
Post-Traumatic Stress Disorder is a reminder of how profoundly trauma can shape the human mind. It is also a testament to the strength of survivors who, even while haunted by memories, continue to fight for healing.
Understanding PTSD means recognizing that it is not a failure of willpower but a natural human response to extraordinary experiences. It requires empathy, science-based treatment, and social support. With the right combination of therapy, medication, and compassion, healing is not only possible but common.
To speak of PTSD is not just to discuss a disorder—it is to acknowledge the invisible battles many people carry, to honor their courage, and to remind them, and ourselves, that recovery is always within reach.