In the vast and intimate theater of the human body, a microscopic drama unfolds every second. Unseen invaders—viruses—slip past our defenses and breach the sanctity of our cells. They are not alive in the traditional sense; they possess no heartbeat, no breath, and no hunger. Yet they are formidable adversaries, capable of hijacking the very essence of life—our genetic machinery—to reproduce and spread.
The moment a virus enters the body, it begins a ruthless campaign. Perhaps it finds entry through a breath inhaled during a crowded subway ride or lingers on a doorknob touched before lunch. It targets vulnerable tissues: the lining of the nose, the throat, or deep within the lungs. Using proteins shaped precisely to match human cellular receptors, the virus latches on and slips inside. Once there, it turns the cell into a factory, churning out copies of itself, flooding the body with viral particles.
But we are not defenseless.
The immune system, honed by millions of years of evolutionary pressure, detects the first signs of invasion with astonishing speed. From the moment the first infected cell sounds the alarm, a cascade of defensive strategies is triggered. The body moves swiftly, calling upon ancient, instinctual responses encoded deep within our DNA. This is the beginning of an invisible war—one that determines whether we get sick, how sick we become, and whether we survive.
The Innate Immune System: Our Ancient First Responder
Long before you realize you’ve been infected—before the sniffles, the fever, the cough—your body has already launched its counterattack. The innate immune system, the body’s oldest and most immediate line of defense, doesn’t need to recognize a virus by name. It doesn’t matter if it’s influenza, Ebola, or the novel coronavirus. It only needs to sense that something is wrong.
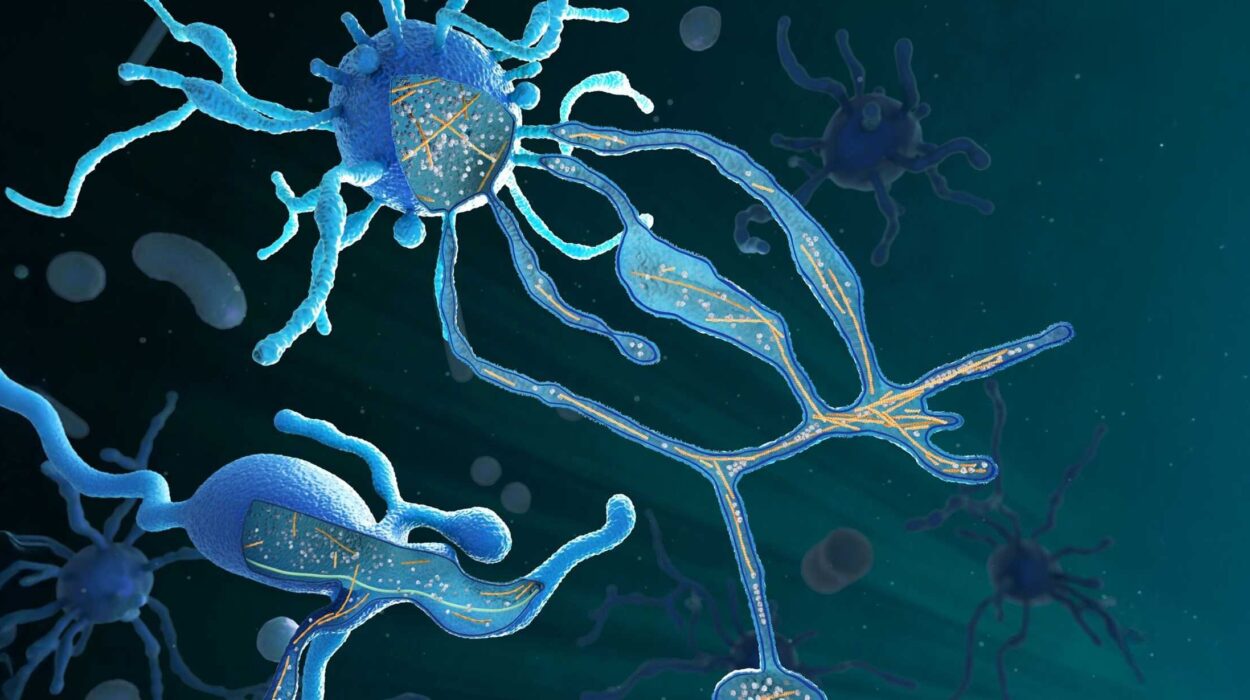
Within minutes of infection, sentinel cells like macrophages and dendritic cells spring into action. They patrol the tissues like microscopic border guards, constantly sampling their environment. When they detect something foreign—like viral RNA or proteins—they engulf it, digest it, and raise the alarm.
One of the most powerful early warning systems comes in the form of cytokines—tiny signaling molecules released in waves that alert neighboring cells and summon immune reinforcements. Among them are interferons, aptly named for their ability to “interfere” with viral replication. These molecules induce an antiviral state in nearby cells, making it harder for the virus to spread.
Neutrophils and natural killer (NK) cells are quickly recruited to the site of infection. Neutrophils, the most abundant white blood cells, attack pathogens directly and release enzymes that damage infected tissues. NK cells are more precise; they detect and destroy virus-infected cells by recognizing subtle changes in the proteins on the cell’s surface.
This initial response can hold the virus at bay, limiting its spread. Sometimes, the innate immune system wins the war before the virus even makes a mark. But often, it’s just the opening act.
The Antigen-Presenting Cells: Translating the Enemy’s Language
As the battle rages, dendritic cells gather pieces of the virus—bits of protein, fragments of genetic code—and migrate to the lymph nodes, the command centers of the immune system. There, they perform a crucial task: presenting the viral antigens to the adaptive immune system, which holds the memory and precision to target the invader specifically.
Antigen-presenting cells are translators in this war. They take the foreign language of the virus and display it in a form that T cells can understand. This interaction is the moment the immune system “learns” what the invader looks like.
Each T cell in the body carries a unique receptor, created randomly, that might recognize a specific antigen. When a T cell encounters a dendritic cell displaying a matching viral fragment, it activates, begins to proliferate, and differentiates into specialized fighters.
The adaptive immune response has been awakened. What follows is a highly coordinated counteroffensive.
Cytotoxic T Cells: The Assassins Within
Among the most fearsome warriors are the cytotoxic T lymphocytes, also known as CD8+ T cells. Once activated, they scour the body for infected cells. Their mission is precise and brutal: identify and destroy cells that have been turned into virus-producing factories.
Infected cells display viral peptides on their surface using molecules called MHC class I. These molecular flags serve as a distress signal. When a cytotoxic T cell recognizes one of these signals, it binds to the infected cell and releases enzymes—perforin and granzymes—that pierce the cell membrane and trigger apoptosis, a form of programmed cell death.
This isn’t random destruction; it’s surgical, targeted, and essential. By sacrificing infected cells, the body prevents the virus from spreading. The collateral damage is contained, and the pathogen’s life cycle is interrupted.
But the cytotoxic T cells aren’t working alone. Another group is preparing a different kind of defense—one that will last a lifetime.
B Cells and Antibodies: Building a Molecular Memory
While T cells are attacking the infected cells, B lymphocytes—another arm of the adaptive immune system—are crafting custom-made weapons. Each B cell carries a receptor on its surface that binds to a specific shape on a virus, like a key fitting a lock. When a B cell finds its match, it becomes activated, often with help from a type of T cell known as a CD4+ helper T cell.
The activated B cell then undergoes a transformation. It multiplies and matures into a plasma cell—a biological factory that produces antibodies at astonishing rates. Antibodies are Y-shaped proteins designed to recognize and bind to the virus with exquisite specificity. Some neutralize the virus directly by blocking its ability to enter cells. Others tag it for destruction, flagging it for immune cells like macrophages to engulf and destroy.
Antibodies are not just weapons. They are memories—lasting molecular signatures of past encounters. Once the infection is cleared, a portion of the B cells becomes memory cells. These cells linger, sometimes for decades, ready to respond within hours if the virus ever returns.
Fever, Fatigue, and Inflammation: The Side Effects of War
While the immune system fights, the body experiences the fallout. Fever rises as the hypothalamus resets the body’s thermostat in response to cytokines. Higher temperatures slow viral replication and boost immune efficiency, but they also leave you feeling weak and chilled.
Fatigue sets in as energy is diverted from muscles to immune function. You may lose your appetite because the body is focusing on battle, not digestion. Swollen lymph nodes, body aches, and headaches are all signs of the war within. They are not symptoms of the virus, but evidence of your immune system doing its job.
Though unpleasant, these symptoms are signs of resilience—a testament to the complexity and strength of your biology. They mean the system is working.
The End of the Battle: Resolution and Recovery
Eventually, the tide turns. The viral load drops. Infected cells are cleared. Antibody levels rise. Memory cells are formed. The inflammation begins to subside. Regulatory T cells help to shut down the immune response, preventing unnecessary damage to healthy tissue.
Tissue repair begins. Damaged epithelial cells in the lungs regenerate. Mucous membranes heal. The immune system, like a well-disciplined army, retreats when the mission is accomplished.
You might be left exhausted, but you are alive—and stronger than before.
Immune Memory: The Secret to Long-Term Protection
One of the most remarkable features of the immune system is its memory. After a viral infection, your immune system remembers the enemy. Memory T cells and B cells persist in your body, standing guard. If the virus ever returns, these cells can reactivate within hours, deploying targeted attacks before the invader can gain a foothold.
This memory is the principle behind vaccines, which train the immune system using harmless pieces or inactivated versions of viruses. A vaccinated immune system is like a well-read soldier—it’s seen the enemy before and knows exactly how to win.
Viral Evasion: The Arms Race Continues
But viruses are clever. Some mutate rapidly, changing their surface proteins to avoid detection. Influenza is infamous for this; it mutates so frequently that new vaccines are needed each year. HIV goes even further, hiding inside cells and attacking the immune system itself. SARS-CoV-2, the virus behind COVID-19, surprised the world by combining traits of contagiousness and immune evasion in ways not fully understood even years after its emergence.
In this eternal arms race between viruses and the immune system, evolution is the battlefield. Viruses adapt to evade immunity. The immune system evolves to recognize new threats. The balance determines not just individual outcomes, but the fate of species.
When the System Fails: Immune Dysfunction and Disease
Sometimes, the immune system misfires. It can overreact, as in a cytokine storm—an uncontrolled flood of inflammatory signals that causes more damage than the virus itself. This has been observed in severe cases of COVID-19 and other viral infections.
Other times, the system underperforms. Immunodeficiencies—whether genetic or acquired—leave the body vulnerable. HIV, for example, targets CD4+ helper T cells, crippling the body’s ability to mount an immune response.
Autoimmune diseases are another kind of failure. In conditions like lupus or rheumatoid arthritis, the immune system mistakenly attacks the body’s own tissues, as if they were foreign invaders.
These disorders underscore how delicate the balance is—how a system so powerful must also be precise.
The Frontier of Immunotherapy and Vaccines
Modern medicine is harnessing the immune system in unprecedented ways. Antiviral drugs are increasingly designed to work alongside the body’s natural defenses. Immunotherapies, such as monoclonal antibodies, give patients ready-made immunity while their own systems catch up.
Vaccines have grown more sophisticated. mRNA vaccines, once theoretical, have now entered reality, delivering instructions directly to cells to build viral proteins and train the immune system with surgical precision.
Scientists are also exploring therapeutic vaccines to fight chronic viral infections like hepatitis B and herpes, and even using viral vectors to teach the immune system to target cancer.
The Immune Symphony: Harmony in Complexity
The immune system is not a single entity but a complex network—a symphony of cells, signals, and structures working in unison. It is both armor and sword, intuition and intelligence. It is capable of destruction but also of exquisite restraint.
It is deeply personal. No two immune systems are alike. Your immune history—shaped by the viruses you’ve encountered, the vaccines you’ve received, your genetics, and even your microbiome—forms an immunological fingerprint as unique as your face.
Every day, your immune system writes a silent story—a story of defense, adaptation, and memory. And though it rarely makes itself known unless something goes wrong, it is always there, standing between you and the invisible world that surrounds us.
Conclusion: The Wisdom of the Body
In a universe teeming with microscopic life, the immune system is our greatest ally. It is at once ancient and cutting-edge, instinctive and learned. Its success is written into every recovered cough, every healed fever, every unnoticed infection that never became an illness.
To understand how the immune system fights viruses is to glimpse the extraordinary power within us. It’s a reminder that survival is not just about fighting; it’s about balance, memory, and the quiet wisdom of the body.
The next time you recover from a cold or stand in line for a vaccine, remember: your immune system has been fighting for you since the day you were born. And every battle it wins is a celebration—not only of life but of the elegant, enduring genius that resides within your cells.