On a brisk February morning in 2025, in a quiet room at Children’s Hospital of Philadelphia (CHOP), a medical revolution quietly unfolded. There were no fanfares, no headlines—just a small baby and a team of scientists and physicians who dared to attempt what many believed was still science fiction. The patient, an infant named KJ, had spent most of his short life tethered to machines, surviving on an impossibly strict diet, and fighting a disease so rare that even seasoned clinicians might never encounter a single case in their careers.
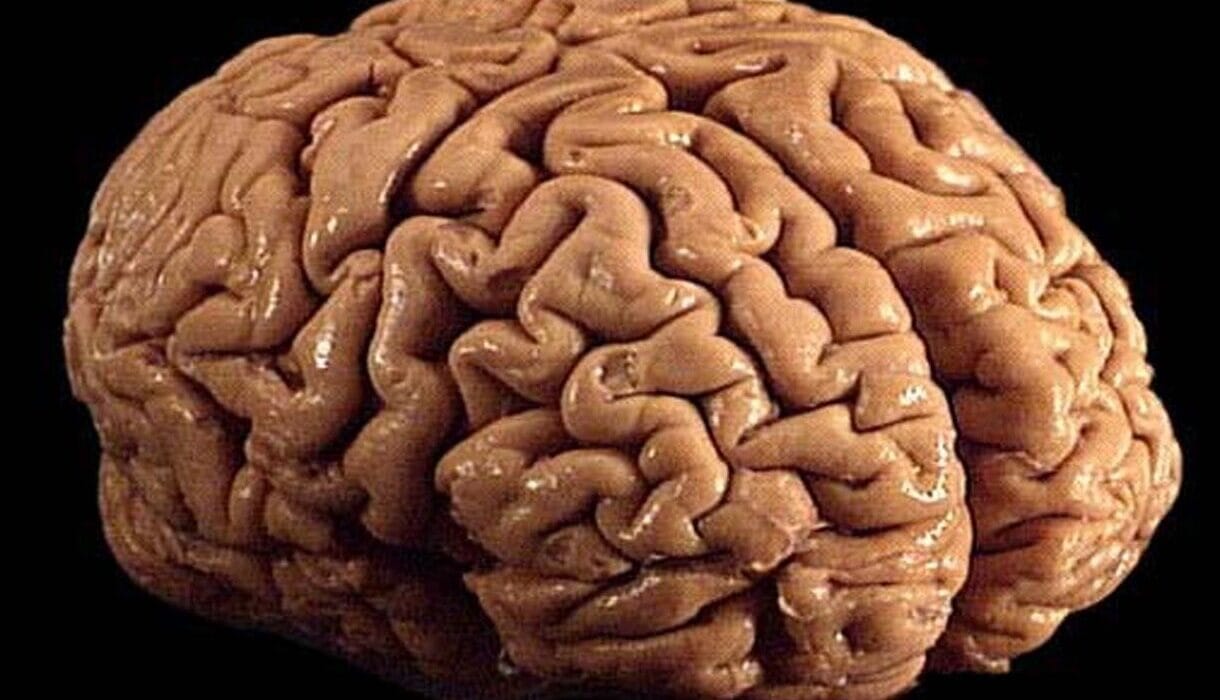
His diagnosis? Severe carbamoyl phosphate synthetase 1 (CPS1) deficiency, a life-threatening genetic disorder of the urea cycle that left his tiny body unable to eliminate ammonia—a toxic byproduct of protein digestion. Without immediate and lifelong intervention, this rare enzyme deficiency leads to neurological damage, coma, and death.
But on that day in February, KJ became the first person to receive a custom-built CRISPR-based gene-editing therapy tailored specifically to his DNA. What happened next may well redefine the future of medicine—not just for KJ, but for millions of patients living with rare genetic diseases once deemed untreatable.
What Is CPS1 Deficiency? A Silent Time Bomb
The urea cycle is one of the body’s most crucial housekeeping systems. Every time we eat protein—whether it’s a glass of milk or a bite of chicken—our body breaks it down into amino acids. These amino acids are then processed in the liver, producing nitrogen. That nitrogen, in the form of ammonia, is highly toxic. For most of us, our liver converts this ammonia into a harmless compound called urea, which is then excreted in urine.
But for KJ, born without a working version of the CPS1 enzyme—the first crucial step in this detox process—that system was broken. Ammonia levels in his blood could spike with any misstep in diet or illness, causing devastating consequences. For many infants born with this condition, life is a constant emergency.
Treatment options are severely limited. A strict low-protein diet and medications known as nitrogen scavengers can help reduce ammonia, but the margin for error is razor-thin. Liver transplant is the only definitive treatment, yet it comes with its own risks, complications, and life-long immunosuppression. There is no cure.
Or rather, there wasn’t.
CRISPR and the Promise of a Genetic Fix
CRISPR, shorthand for clustered regularly interspaced short palindromic repeats, is often likened to molecular scissors. But in reality, it’s more like a GPS-guided precision editing tool, capable of locating specific mutations in the vast landscape of the human genome and rewriting them.
This technology, barely a decade old, has already made waves. In 2023, the first CRISPR-based therapies for sickle cell disease and beta thalassemia were approved in the U.S., marking a historic moment in medicine. But those therapies targeted mutations common to tens of thousands of patients worldwide. What about the vast majority of rare diseases—those affecting only a handful of children like KJ?
For these patients, a one-size-fits-all model doesn’t work. Each genetic error is often unique, making standardization difficult and pharmaceutical investment rare. That’s where the approach by CHOP and Penn Medicine stood out: a truly personalized gene editing therapy, built not for a population, but for a single child.
From Diagnosis to Delivery: Designing a Therapy in Real Time
The effort to treat KJ was led by two pioneers in their respective fields: Dr. Rebecca Ahrens-Nicklas, director of the Gene Therapy for Inherited Metabolic Disorders Frontier Program at CHOP, and Dr. Kiran Musunuru, a renowned geneticist at Penn’s Perelman School of Medicine.
Their collaboration began in 2023, spurred by a mutual belief that the most powerful tools in medicine should not be reserved only for common conditions. They focused on urea cycle disorders, among the most dramatic and medically demanding of all metabolic diseases.
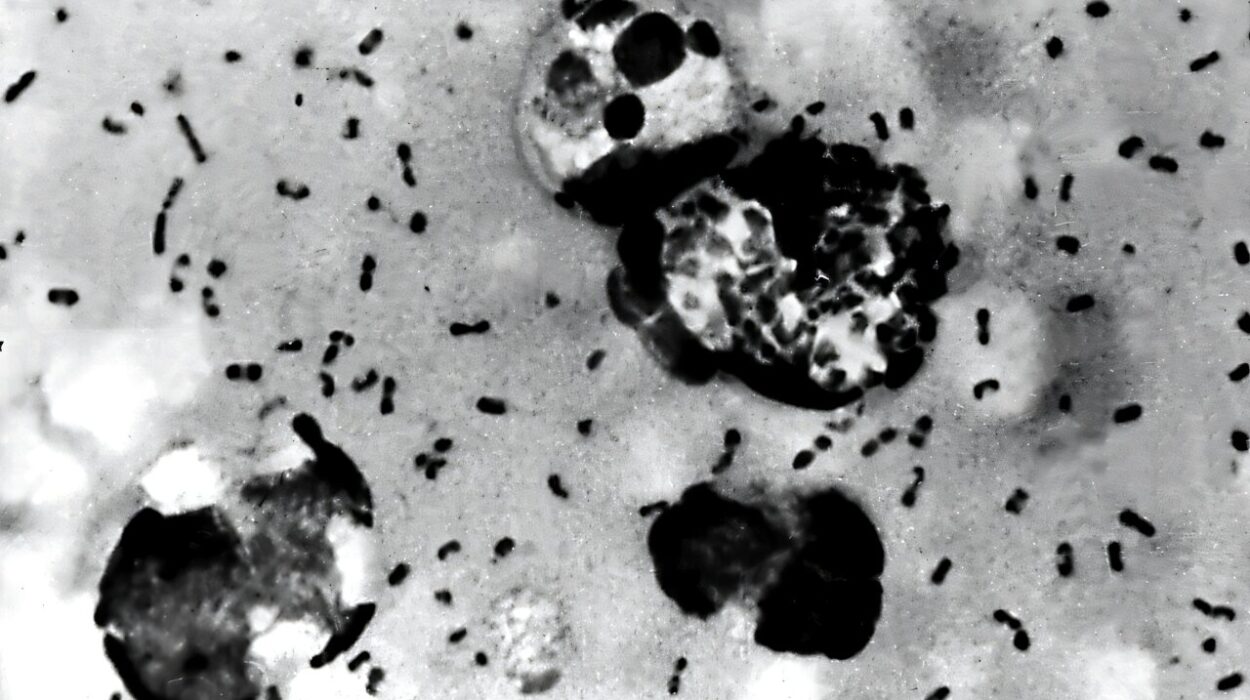
When KJ was diagnosed shortly after birth, his genetic sequencing revealed a specific mutation in his CPS1 gene. Within weeks, Ahrens-Nicklas and Musunuru’s team began designing a bespoke base-editing therapy—a CRISPR variant capable of making precise single-letter changes to DNA, without cutting both strands of the double helix, thereby reducing potential side effects.
The delivery vehicle of choice? Lipid nanoparticles, tiny fat-based bubbles engineered to deliver gene-editing payloads directly to the liver, where the CPS1 enzyme is made. This method avoids the use of viral vectors, reducing long-term risks and offering the possibility of repeated doses if needed.
By February 2025—just six months after initiating the design process—KJ received his first infusion. Over the next two months, he received two more doses, all without serious side effects.
Measuring the Impact: A Life Reclaimed
Within weeks, the changes were dramatic. KJ began tolerating more protein in his diet, a once-impossible goal. He required lower doses of nitrogen scavenger medications. When he contracted rhinovirus—a common childhood illness that would typically trigger a metabolic crisis—his ammonia levels remained stable.
These early signs were more than encouraging; they were extraordinary. For a child who had once teetered on the edge of metabolic catastrophe, KJ was now growing, smiling, and hitting developmental milestones.
The team published the case in The New England Journal of Medicine and presented it at the American Society of Gene & Cell Therapy Annual Meeting in New Orleans. The case wasn’t just a triumph of clinical execution; it was a roadmap for others.
A New Model for Rare Disease Therapy
Rare diseases affect over 300 million people worldwide, yet fewer than 5% have FDA-approved treatments. Part of the challenge lies in the diversity and individuality of these disorders. But what if each patient could receive a therapy built just for them?
This is the vision now coming into focus: ultra-personalized medicine, in which CRISPR therapies can be custom-designed within months to target a unique mutation, manufactured in academic or biotech labs, and safely administered under compassionate-use frameworks.
Of course, this approach is not without challenges. The costs of developing individualized therapies are high, the regulatory pathways complex, and long-term outcomes still unknown. But the case of KJ shows that such a model is possible—and that academic institutions, with the right partnerships, can lead the way.
The Ethics of Editing: Where Science Meets Humanity
As this new frontier opens, so too do ethical questions. How do we ensure equitable access to customized therapies? Will only the wealthy benefit from precision medicine, or can public funding and academic innovation democratize access?
There are also deeper questions about the nature of gene editing itself. When is it appropriate to intervene? How do we define safety and efficacy when dealing with one patient at a time? What kind of long-term monitoring will be necessary?
For Ahrens-Nicklas and Musunuru, the answers begin with transparency, rigorous oversight, and a commitment to doing what’s best for the patient. “We want each and every patient to have the potential to experience the same results we saw in this first patient,” said Musunuru. “We hope other academic investigators will replicate this method for many rare diseases and give many patients a fair shot at living a healthy life.”
The Road Ahead: A Revolution in Motion
The success of KJ’s treatment is not the end of the story—it’s the beginning of a new one. Already, other teams are exploring similar strategies for rare metabolic and neurological diseases. Tools like base editing and prime editing are evolving rapidly, offering even more precision and flexibility.
Meanwhile, advances in AI, machine learning, and high-throughput sequencing are making it faster and cheaper to identify mutations, predict pathogenicity, and design corrective edits. What once took years in the lab can now happen in weeks.
In this evolving landscape, gene editing is not just about fixing broken genes. It’s about changing the way we understand and practice medicine. It moves the field from a reactive posture—treating symptoms—to a proactive one: rewriting the very blueprint of disease.
One Small Life, One Giant Leap for Medicine
Baby KJ may never fully understand the role he played in medical history. To him, this story will be one of ordinary love, of parents who fought for him, doctors who believed in him, and science that saved him.
But to the rest of us, it marks a watershed moment—a glimpse into a future where rare diseases are no longer death sentences, but puzzles to be solved, one patient at a time.
In the words of Dr. Ahrens-Nicklas: “Years and years of progress in gene editing and collaboration between researchers and clinicians made this moment possible. While KJ is just one patient, we hope he is the first of many.”
And in that hope, we see the birth of a new kind of medicine—personal, precise, and profoundly human.
Reference: Musunuru et al, Patient-Specific In Vivo Gene Editing to Treat a Rare Genetic Disease, New England Journal of Medicine (2025). DOI: 10.1056/NEJMoa2504747