In the not-so-distant past, medical diagnostics was largely dependent on the intuition, memory, and training of human physicians. A sharp eye, a steady hand, and years of experience could mean the difference between life and death. Radiologists pored over X-rays with magnifying glasses, pathologists examined tissue under microscopes, and clinicians compared symptoms to textbook cases. But today, something extraordinary is happening. Machines—not just any machines, but artificial intelligence (AI)—are rapidly transforming the way we diagnose disease.
This is not just a technological upgrade. It is a profound paradigm shift, akin to the invention of the microscope or the discovery of antibiotics. AI is now analyzing images, reading genomic sequences, flagging abnormalities in electronic health records, and, in some cases, outperforming experienced doctors in identifying diseases. From radiology suites to primary care offices, AI is infiltrating the diagnostic process with speed, accuracy, and a kind of digital intelligence that promises to revolutionize the practice of medicine.
In this article, we’ll explore how AI is reshaping medical diagnostics, the technologies driving this revolution, the benefits and challenges, and what the future might hold. Through stories, science, and speculation, we’ll uncover why AI is not just a tool but a partner in medicine’s most critical mission: understanding what’s wrong—and how to fix it.
The Foundation: What Exactly Is AI in Diagnostics?
Artificial intelligence, at its core, refers to the development of computer systems capable of performing tasks that typically require human intelligence. In diagnostics, this involves algorithms trained to recognize patterns in complex data—whether images, sounds, numbers, or language.
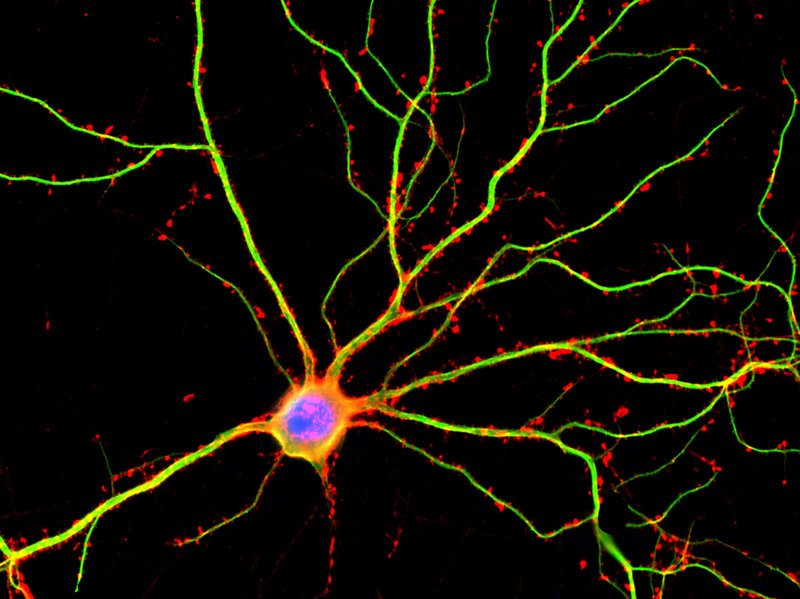
The most common form of AI in diagnostics today is machine learning (ML), particularly deep learning—a technique inspired by the human brain’s network of neurons. Deep learning models, especially convolutional neural networks (CNNs), are exceptionally good at interpreting visual data, making them ideal for medical imaging tasks. Others, like recurrent neural networks (RNNs), are better at understanding sequences and time-series data, such as heart rhythms or patient histories.
These systems are trained using massive datasets: thousands or millions of labeled examples of diseases, images of healthy and unhealthy organs, genomic sequences, and more. As the algorithm sees more examples, it “learns” to detect subtle patterns, correlations, and anomalies that may be imperceptible to the human eye. Once trained, these models can analyze new data in real time, offering diagnostic suggestions or red-flagging abnormalities for human review.
But AI doesn’t operate in a vacuum. Its real-world use depends on integration with existing clinical workflows, compatibility with electronic health records (EHRs), and, above all, collaboration with human healthcare professionals.
Radiology: The First Frontier of AI Diagnostics
If there is one area where AI has already made a significant mark, it is radiology. Medical imaging generates immense volumes of data—X-rays, CT scans, MRIs, ultrasounds—all of which require careful interpretation. Radiologists are tasked with identifying tumors, fractures, infections, blood clots, and other abnormalities, often under pressure and with limited time.
AI has proven particularly adept at image recognition. Deep learning models trained on tens of thousands of chest X-rays can now detect signs of pneumonia, tuberculosis, lung cancer, or COVID-19 with accuracy comparable to or exceeding that of experienced radiologists. AI can spot subtle differences in texture, density, and shape that might escape the human eye—especially in the early stages of disease when intervention is most effective.
One notable example is the use of AI in mammography. Breast cancer screening involves analyzing mammograms for masses or calcifications that could indicate tumors. False positives are common, leading to unnecessary biopsies and anxiety. AI systems have been trained to distinguish benign from malignant features, reducing both false positives and false negatives. Studies have shown that AI-assisted diagnosis in mammography can improve detection rates, especially in dense breast tissue where tumors are harder to detect.
In brain imaging, AI is aiding in the detection of stroke and hemorrhage in emergency settings, often identifying abnormalities within seconds—crucial when every minute of delayed treatment increases the risk of brain damage. In orthopedics, AI is helping detect subtle fractures. In oncology, AI can map the exact boundaries of tumors to guide surgical or radiological intervention.
Importantly, AI in radiology is not replacing radiologists but augmenting them. A radiologist working with AI is faster, more accurate, and less prone to fatigue. This collaboration between human and machine, often called “augmented intelligence,” represents the most promising future for diagnostics.
Pathology and Histology: A Digital Microscope with a Brain
Another critical domain where AI is transforming diagnostics is pathology, the microscopic examination of tissues and cells to diagnose disease. Traditionally, pathologists manually examine biopsy samples under a microscope, identifying cellular structures and patterns associated with disease states. It is meticulous, painstaking work, and subject to inter-observer variability.
Enter digital pathology. With the advent of high-resolution slide scanners, pathology slides can now be digitized, stored, and analyzed by AI systems. These models can detect cancerous cells, grade tumors, and even predict prognosis based on histological features. AI is particularly useful in prostate, breast, and skin cancer diagnosis, where subtle morphological differences can be diagnostically significant.
One breakthrough application has been in melanoma detection. Dermatopathologists must distinguish between benign moles and malignant melanomas, a task complicated by the wide variability in appearance. AI algorithms trained on thousands of labeled skin images can classify lesions with remarkable precision, often surpassing dermatologists in controlled studies.
Furthermore, AI is being used to quantify features like mitotic rate, cellular density, and vascular invasion—details that are often difficult to measure consistently by human eye but are crucial for determining treatment plans. Some systems can even analyze immunohistochemical stains to assess protein expression levels, guiding personalized therapies in oncology.
As with radiology, AI in pathology doesn’t eliminate the need for human experts. Instead, it acts as a second set of eyes, flagging suspicious areas on slides, triaging normal versus abnormal samples, and helping standardize interpretations. It accelerates workflow and reduces diagnostic errors—especially in resource-limited settings where experienced pathologists are in short supply.
Genomics and Precision Medicine: AI Meets Big Biology
Perhaps the most futuristic application of AI in diagnostics lies in the field of genomics—the analysis of DNA and RNA to understand disease at its most fundamental level. With the plummeting cost of genome sequencing, clinicians now have access to vast amounts of genetic data. But sifting through billions of base pairs to find clinically relevant mutations is like looking for needles in haystacks the size of mountains.
This is where AI becomes indispensable. Machine learning models can analyze genomic sequences to identify pathogenic mutations, detect hereditary disease risk, and even guide cancer treatment based on tumor genetics. AI systems can predict how mutations affect protein function, assess the likely impact of noncoding variants, and integrate genomic data with clinical history to offer a probabilistic diagnosis.
In rare genetic diseases, AI tools like phenotype matching have proven game-changing. These systems compare a patient’s symptoms, lab results, and genetic variants with databases of known disorders, narrowing down possible diagnoses that would take a human geneticist weeks to consider.
In cancer genomics, AI helps interpret liquid biopsy data—DNA fragments shed by tumors into the bloodstream. By analyzing mutation patterns, methylation signatures, and gene expression profiles, AI can detect cancer at early stages or monitor its progression non-invasively.
This convergence of AI and genomics fuels the dream of precision medicine—tailoring treatment to the individual’s unique genetic makeup. By diagnosing disease at the molecular level, we move beyond the one-size-fits-all model and toward therapies that are safer, more effective, and more targeted than ever before.
Primary Care and Electronic Health Records: AI as a Diagnostic Assistant
Not all diagnostic challenges happen in high-tech labs or imaging suites. In primary care, where general practitioners see a wide range of conditions with limited time and resources, AI is beginning to serve as a clinical co-pilot.
AI-driven decision support systems can analyze a patient’s symptoms, history, lab results, and even socio-demographic data to suggest possible diagnoses. Some tools, like symptom checkers and chatbots, engage directly with patients before they see a doctor, triaging complaints and recommending next steps.
Perhaps most powerful is the integration of AI with electronic health records (EHRs). These digital repositories contain a goldmine of diagnostic information—medications, lab results, imaging reports, clinical notes—but often suffer from clutter and inconsistency. AI algorithms can sift through these records, identifying patterns of concern (e.g., early signs of diabetes, cardiovascular risk, drug interactions) and prompting clinicians to investigate further.
Natural language processing (NLP), a branch of AI focused on understanding human language, is especially important here. NLP can extract relevant information from unstructured clinical notes—something conventional data systems struggle with—and turn it into actionable insights.
In emergency settings, AI can help diagnose conditions like sepsis or acute kidney injury by continuously monitoring vitals and labs, alerting clinicians before symptoms become obvious. This predictive capability is a major leap forward, turning diagnostics from reactive to proactive.
The Human Side: Ethics, Bias, and Trust in AI Diagnostics
Despite its enormous potential, AI in diagnostics is not without challenges. Among the most pressing concerns is bias. AI systems learn from data, and if that data reflects historical biases—such as racial disparities in healthcare—they can perpetuate or even amplify these inequities. An algorithm trained mostly on images of light-skinned patients, for instance, may perform poorly on darker-skinned individuals. Such blind spots are unacceptable in medical care.
Transparency is another issue. Many AI models, especially deep learning networks, operate as “black boxes,” making decisions that are difficult to explain. In a field where trust, accountability, and informed consent are paramount, this opacity can be problematic. Patients and physicians alike need to understand why an AI made a particular recommendation.
There is also the question of responsibility. If an AI system makes a wrong diagnosis, who is liable? The developer? The healthcare provider? The institution? Regulatory bodies are grappling with these questions as AI becomes more integrated into clinical practice.
Importantly, there is the human dimension: trust. Physicians are trained not only to diagnose but to communicate, empathize, and make judgments based on experience and ethics. Patients seek more than answers—they seek reassurance. AI cannot replace this human connection, but it can support it, allowing doctors to spend more time with patients and less on administrative burden.
Looking Ahead: The Future of AI-Powered Diagnostics
The future of AI in diagnostics is both thrilling and complex. As computational power increases and data grows richer, we can expect even more sophisticated diagnostic tools—AI that integrates images, genetics, clinical history, and real-time data from wearable devices to offer truly holistic assessments.
We may soon see AI-powered diagnostic kiosks in pharmacies, enabling rapid screening for common ailments. Mobile apps may allow people in remote areas to self-scan moles or listen to their heartbeat, with AI providing preliminary evaluations. AI may even help decode the diagnostic clues hidden in a person’s voice, gait, or facial expression.
In hospitals, AI will become a constant companion—monitoring patients around the clock, flagging deterioration, predicting complications, and coordinating care. In research, AI will help uncover new disease subtypes and biomarkers, enabling earlier and more accurate diagnoses.
But amid this high-tech revolution, the soul of medicine must remain human. The physician’s role will evolve—from sole diagnostician to interpreter, mediator, and caregiver in a data-rich landscape. The best outcomes will arise not from man or machine alone, but from their collaboration.
Conclusion: Intelligence Augmented, Not Replaced
Artificial intelligence is not replacing doctors; it is augmenting them. In diagnostics, this augmentation is already saving lives, speeding care, reducing errors, and expanding access. AI doesn’t get tired, distracted, or forgetful. But it also doesn’t feel, understand context, or make moral decisions. That’s where humans remain irreplaceable.
Together, AI and humans are creating a new medical paradigm—one where machines handle complexity, crunch data, and spot patterns, while people do what they do best: care, connect, and heal. In this partnership lies the future of diagnostics—and perhaps, the future of medicine itself.