In a groundbreaking study, scientists at UCLA Health have peeled back the layers of one of the most puzzling neurological riddles of our time: why certain children with a rare genetic disorder are more likely to develop autism or schizophrenia. By tracing changes in brain connectivity across critical developmental stages, researchers have illuminated a potential biological mechanism that may drive these psychiatric disorders—offering hope for new treatment pathways and early interventions.
The study, recently published in Science Advances, takes a closer look at chromosome 22q11.2 deletion syndrome—a condition caused by the loss of a small piece of DNA on chromosome 22. While this deletion is rare, its effects are profound: individuals with the syndrome are up to 25 times more likely to develop schizophrenia and significantly more likely to show traits associated with autism. But what is it about this missing genetic material that disrupts the developing brain?
Until now, scientists have lacked clear insight into the biological basis of this elevated risk. However, by integrating human brain imaging with mouse model studies, the UCLA-led team uncovered something striking: the pattern of brain connectivity in individuals with the 22q11.2 deletion dramatically changes at puberty, and this shift might be the key to understanding the associated neuropsychiatric risk.
Before and After Puberty: A Tale of Two Brain States
Before puberty, both human patients and genetically engineered mice with the 22q11.2 deletion exhibited hyperconnectivity in specific regions of the brain. These are not just any regions—they are the very areas linked to social cognition and behavior, which are central to both autism and schizophrenia.
But something remarkable happens during puberty. The once-overactive connections become under-connected—a stark reversal that mirrors the age at which many neuropsychiatric symptoms begin to emerge in affected individuals.
“This dramatic shift in brain connectivity was one of the most compelling findings of our study,” said Dr. Carrie Bearden, a professor at UCLA’s Semel Institute for Neuroscience and Human Behavior and co-senior author of the study. “It suggests that something fundamental is changing at the synaptic level during this developmental window.”
Zooming In: What’s Happening at the Synapse?
To understand what might be causing this flip in brain activity, the team turned to the building blocks of neural communication—synapses—specifically, the tiny protrusions on neurons known as dendritic spines. These structures serve as communication hubs between brain cells, and their density is a powerful indicator of synaptic activity.
In the pre-pubertal phase, mice with the 22q11.2 deletion had a higher-than-normal density of dendritic spines, indicating heightened synaptic activity. But after puberty, the spine density plummeted far below that of normal mice, suggesting a process of aggressive synaptic pruning—essentially, an overzealous cleanup that may be scrubbing away too many critical connections.
This over-pruning could be at the heart of the reduced brain connectivity observed in adolescence and early adulthood—and may explain the sudden emergence of social and cognitive symptoms around the same time.
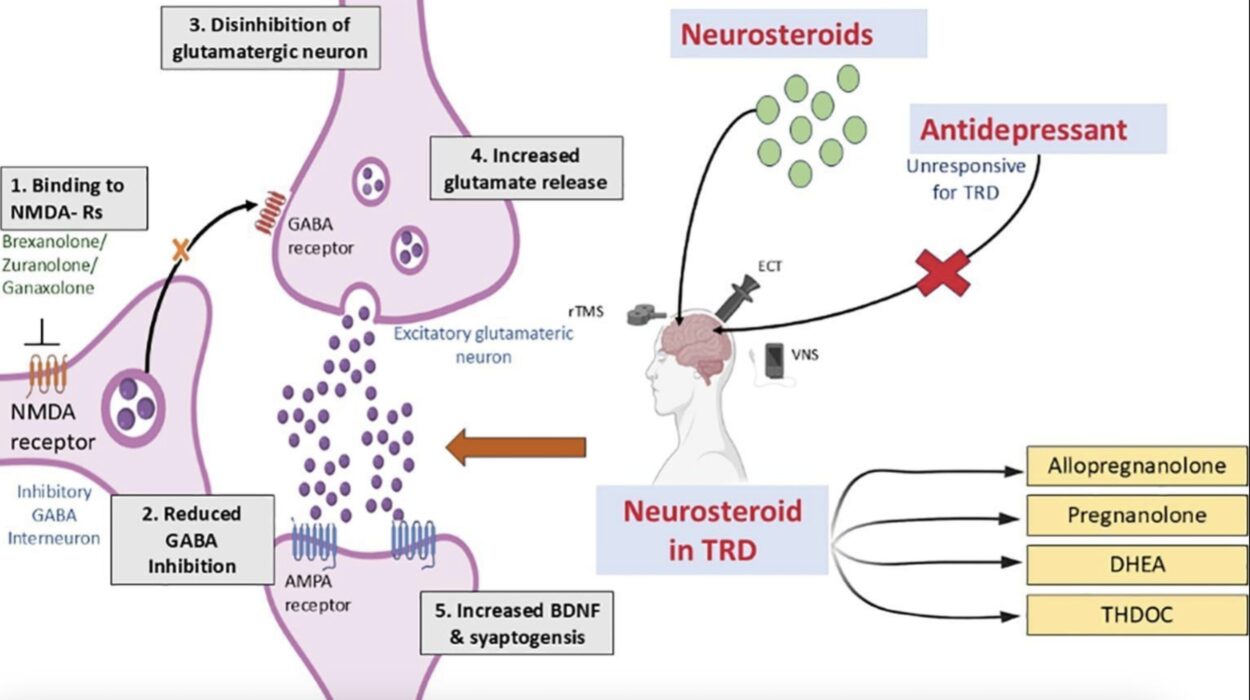
The GSK3-Beta Puzzle Piece
One of the most exciting aspects of this research is the identification of a potential molecular culprit: GSK3-beta, a protein known to be involved in synaptic regulation and neural plasticity. Intriguingly, brain regions affected by connectivity changes in humans with 22q11.2 deletion were enriched in genes associated with GSK3-beta.
The researchers took the next logical step: what happens if you block this protein’s activity? In mice, using a drug to inhibit GSK3-beta not only restored dendritic spine density but also reactivated normal patterns of brain activity—at least temporarily.
“Modulating GSK3-beta might offer a way to slow or even reverse some of the synaptic dysfunctions,” Dr. Bearden explained. “It’s an early but promising step toward possible therapeutic strategies.”
From Mouse to Mind: What This Means for Humans
One of the remarkable aspects of this study is how tightly the human and mouse data lined up. Using functional MRI scans, researchers saw that the same patterns of brain hyperconnectivity and later under-connectivity occurred in people with the 22q11.2 deletion. And just like in the mice, these connectivity changes correlated strongly with social behavior difficulties, a hallmark of autism spectrum disorder.
This cross-species validation is rare and powerful, providing compelling evidence that the same biological mechanism—a misregulation of synaptic pruning—is at play in both animals and humans.
Moreover, the timing of these changes underscores the critical role of puberty as a window of vulnerability. It’s during this stage that the brain is sculpting itself for adulthood. If too many synapses are pruned—or the wrong ones—the result may be long-term disruptions in the neural circuits responsible for social reasoning, emotional regulation, and cognitive flexibility.
A Glimpse Toward the Future
The implications of this study are far-reaching. First, it highlights the importance of developmental timing in understanding psychiatric illness. Disorders like autism and schizophrenia don’t appear overnight—they unfold gradually, often beginning with subtle changes in brain connectivity long before symptoms emerge.
Second, the study offers new leads for targeted interventions. If researchers can identify children at risk—through genetic screening or early brain imaging—it may be possible to intervene during the pre-pubertal window, before the pruning process begins in earnest.
“This is a moment of opportunity,” Dr. Bearden emphasized. “By understanding the biological mechanisms during brain development, we have a chance to change the trajectory of these conditions.”
Bridging the Gap Between Genes and Behavior
While chromosome 22q11.2 deletion syndrome affects only a small number of people, the mechanisms uncovered in this study may generalize to broader populations. Many psychiatric disorders, including autism and schizophrenia, are believed to involve dysregulation of synaptic pruning and connectivity during adolescence.
That means this research could inform our understanding of more common forms of these disorders and pave the way for novel treatment strategies across a range of conditions.
In a world where brain disorders are often diagnosed only after symptoms have become disruptive or debilitating, this study represents a paradigm shift—a movement toward biological early detection, developmentally timed treatments, and precision medicine tailored to the individual’s unique neural and genetic profile.
Conclusion: A New Map of the Mind
The UCLA-led study delivers more than just a new understanding of a rare genetic condition. It provides a blueprint for decoding the brain’s most complex disorders by focusing on the dynamic changes that occur across development. Through a powerful combination of imaging, genetics, and animal models, researchers have identified a potential root cause of connectivity changes tied to psychiatric illness—and offered the tantalizing possibility that these changes can be modulated or even reversed.
In the process, they’ve not only brought us one step closer to unraveling the mystery of autism and schizophrenia but also opened a new chapter in our ongoing quest to understand the most mysterious organ of all: the human brain.
Reference: Filomena Grazia Alvino et al, Synaptic-dependent developmental dysconnectivity in 22q11.2 deletion syndrome, Science Advances (2025). DOI: 10.1126/sciadv.adq2807