In a world where mental health issues are often reduced to just emotional or psychological struggles, a groundbreaking discovery has shifted the way we understand depression. A team of researchers from KAIST has revealed that depression may not simply be a problem confined to the mind or brain but is instead deeply connected to the body’s immune response. This unexpected link between mental health and the immune system is not just a revelation—it could change everything about how we diagnose and treat depression.
The findings, published in the prestigious journal Advanced Science, illuminate how the body’s immune system and the brain are interconnected in a delicate, often broken, balance in individuals suffering from Major Depressive Disorder (MDD). According to the research, it’s not just the brain’s chemistry at play, but a complex imbalance in the immune system that might be at the heart of depression, opening up the possibility for new biomarkers and novel treatments.
Uncovering a Hidden Connection
Major Depressive Disorder (MDD) is a serious mental health condition that affects millions of people worldwide, causing a profound loss of interest in daily activities, severe mood disturbances, and in extreme cases, suicidal thoughts. But despite its prevalence, depression is notoriously difficult to diagnose and treat. There are currently no objective biological markers to confirm a diagnosis or guide treatment, leaving many people to suffer without clear answers.
Professor Jinju Han, who led the research team from KAIST’s Graduate School of Medical Science and Engineering, joined forces with Professor Yangsik Kim from Inha University School of Medicine to examine a particularly puzzling subset of patients: young women with MDD who show atypical features. These individuals, who often struggle with hypersomnia (excessive sleep), overeating, mood reactivity, and psychotic symptoms such as auditory hallucinations or extreme guilt, are frequently misdiagnosed or overlooked. They also tend to have impaired reality judgment, complicating their diagnosis further.
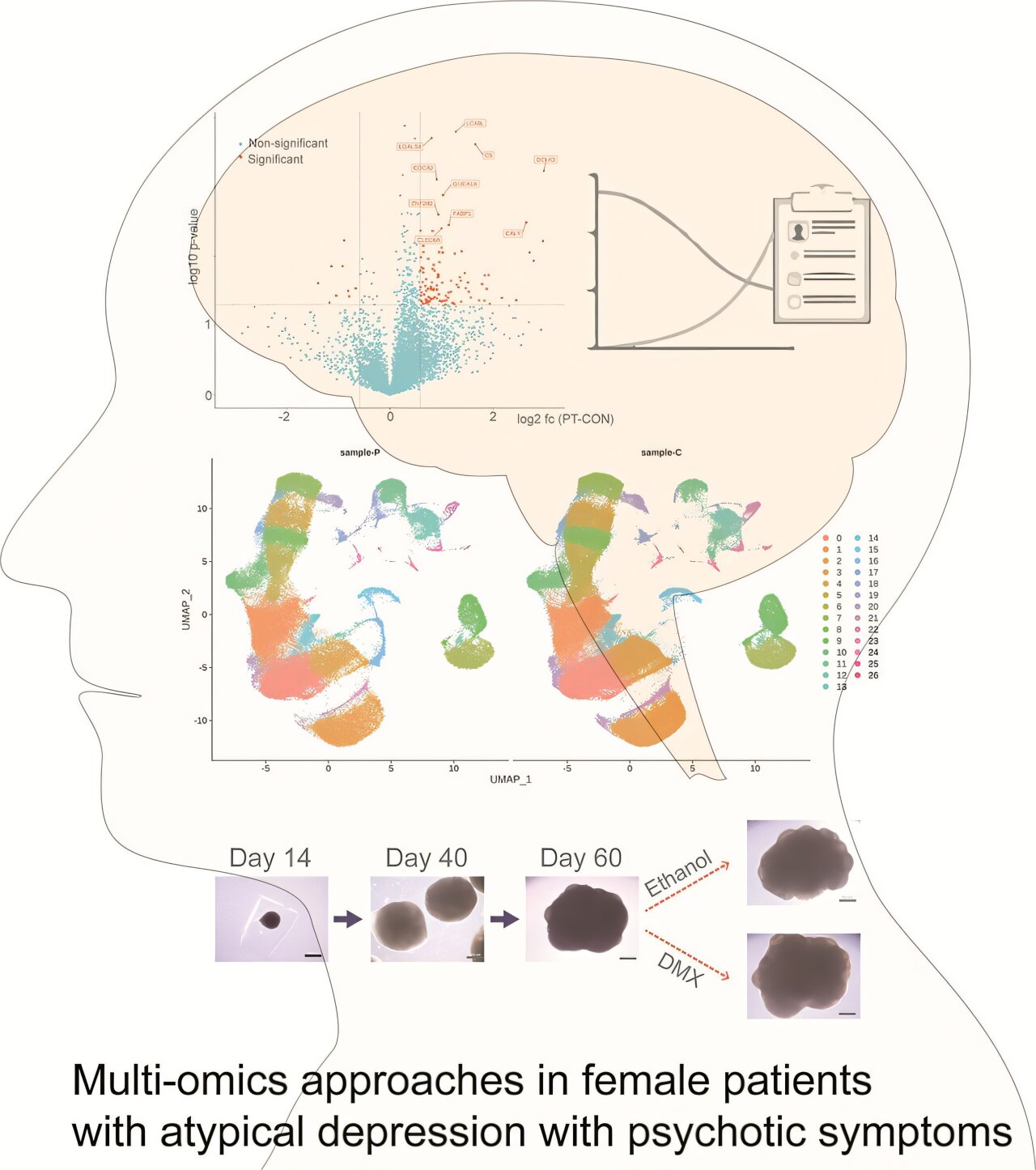
Through a multi-layered analysis involving blood tests, single-cell studies, and brain organoids (miniature brains grown in the lab from patient-derived cells), the team discovered something remarkable. They found a breakdown in the immune system’s delicate balance—a disruption that affects not only immune cells in the blood but also neural pathways in the brain. This breakdown, the researchers concluded, is central to the development of depression.
Immune Cells and the Brain’s Response
The research team didn’t just focus on the brain, as most studies on depression do. They looked at the whole body—specifically at immune cells in the blood and changes in brain-related proteins. What they found was a stunning connection: the immune system and brain function are altered together in people suffering from depression.
More specifically, the study revealed that in those with atypical depression, there is an excessive activation of both immune responses and brain function. Certain proteins crucial for neural signaling, like DCLK3 and CALY, were found to be significantly elevated in depressed patients. These proteins play an essential role in how neurons communicate with one another, and their heightened levels suggest that the brain’s signaling processes are on overdrive.
Meanwhile, Complement Protein C5, which typically enhances the body’s immune response during inflammation, was also increased, pointing to an immune system that is excessively activated. This imbalance between immune and neural activity is what the researchers believe underlies the progression of depression.
The findings suggest that depression isn’t just a mood disorder or a brain malfunction but is deeply rooted in the immune system’s reaction to stress and inflammation. The immune system, in this case, seems to be out of sync with the brain, amplifying both physical and psychological symptoms.
The Bigger Picture: A New Approach to Psychiatric Research
One of the most revolutionary aspects of this study is how it introduces a new model of psychiatric research. By integrating plasma proteomics (the study of proteins in blood), single-cell transcriptome analysis of immune cells, and brain organoids derived from patient stem cells, the researchers have developed what they call a “precision medicine” approach. This approach combines the latest tools in genomics, cell biology, and neuroscience to gain a more comprehensive understanding of depression.
The results point to a crucial insight: depression, especially in its atypical form, may not be a simple brain issue but rather a complex, body-wide disruption. The immune system’s hyperactivity, which can cause inflammation throughout the body, may also be damaging brain function, leading to the hallmark symptoms of depression. This new perspective opens up possibilities for targeting the immune system as a treatment strategy, a shift away from the traditional focus on antidepressants that only address brain chemistry.
For Professor Jinju Han, this represents a monumental step forward. “This achievement presents a new precision medicine model for psychiatric research,” she said. “We anticipate that this will actively lead to biomarker discovery and new drug development.”
Why This Research Matters
What makes this research so important is that it doesn’t just suggest a new theory—it offers a practical path forward. Major Depressive Disorder, particularly in young women, is notoriously difficult to treat, with many patients showing no response to traditional antidepressants. In fact, approximately 40% of those suffering from depression are classified as “treatment-resistant,” meaning they don’t benefit from the usual therapies.
By pinpointing immune system irregularities as a key factor in the development of depression, this research opens the door to new therapeutic strategies. Instead of relying solely on antidepressants, doctors could soon have access to treatments that target the immune system, potentially offering relief to patients who don’t respond to current options.
Moreover, the study’s focus on precision medicine—tailoring treatment to the specific biological factors at play in an individual’s depression—could lead to more personalized, effective interventions. This means better outcomes for patients and a deeper understanding of the biology of depression that could transform both diagnosis and treatment in the future.
The significance of this research cannot be overstated. Depression is a silent epidemic, with far-reaching effects on both individuals and society. It is linked to diminished quality of life, impaired work and academic performance, and, in many tragic cases, suicide. In South Korea, where suicide rates are among the highest in the world, the impact of depression cannot be ignored.
This discovery offers hope—hope for better diagnosis, better treatment, and, ultimately, a better quality of life for those suffering from one of the most common and debilitating mental health conditions of our time.
More information: Insook Ahn et al, Exploration of Novel Biomarkers Through a Precision Medicine Approach Using Multi‐Omics and Brain Organoids in Patients With Atypical Depression and Psychotic Symptoms, Advanced Science (2025). DOI: 10.1002/advs.202508383