The human immune system is one of the most astonishing and misunderstood systems in the body. It is invisible, tireless, and relentlessly vigilant, working every second of every day to keep us alive. Most of the time, we only notice it when it fails—when we get sick, develop allergies, or suffer from autoimmune disease. Yet beneath the surface, the immune system is performing feats so complex and strange that for centuries they baffled scientists.
Why does the body sometimes attack itself? How can it remember infections from decades ago? Why do some people never get sick while others catch everything? These questions once lived in the realm of mystery. Thanks to modern science, many of them now have answers—answers that reveal a system more intelligent, emotional, and adaptive than we ever imagined.
Here are ten of the greatest mysteries of the human immune system, finally explained.
1. How the Immune System Knows What Belongs to You
One of the most profound mysteries in biology is how the immune system distinguishes between “self” and “non-self.” Your body contains trillions of cells, all carrying molecules that mark them as yours. At the same time, bacteria, viruses, and parasites constantly try to invade, wearing molecular signatures that are subtly different.
The immune system solves this problem through a sophisticated recognition process. Immune cells are trained early in life to recognize your body’s own molecular patterns, particularly proteins found on the surface of cells. This training occurs in specialized organs where immune cells that react too strongly to “self” are eliminated or reprogrammed.
This process is not perfect, but it is astonishingly effective. Every day, immune cells scan your tissues, touching and testing other cells, searching for signs of danger. When they encounter something unfamiliar or altered, such as a virus-infected cell or a cancerous mutation, they respond with precision.
This ability to recognize “you” is not learned consciously—it is encoded through evolutionary refinement and biological education. It is the foundation of immunity and one of the most elegant solutions nature has ever devised.
2. Why You Can Get the Same Illness Only Once (Sometimes)
Why does chickenpox usually strike only once, while the common cold keeps coming back? For generations, this seemed mysterious. The answer lies in immune memory.
When your immune system encounters a pathogen for the first time, it launches a massive response. Specialized cells learn the invader’s molecular features and store this information. Some of these cells become long-lived memory cells, capable of surviving for decades.
If the same pathogen returns, memory cells recognize it almost instantly. The immune response is faster, stronger, and more targeted, often stopping the infection before symptoms appear. This is why many childhood diseases rarely return.
However, not all pathogens play by the same rules. Some viruses, like those that cause colds or influenza, mutate rapidly. Each new version looks different enough to fool immune memory, forcing the immune system to start over again.
This balance between memory and mutation explains why immunity can last a lifetime—or vanish in a season. It also explains the power of vaccines, which train immune memory without the danger of disease.
3. Why the Immune System Sometimes Attacks the Body Itself
Autoimmune diseases once seemed like cruel accidents of nature. Why would a system designed to protect us turn against us? The answer lies in the complexity of immune tolerance.
During immune development, cells that strongly recognize “self” are usually destroyed. But this process is not absolute. Some self-reactive cells slip through, kept under control by regulatory immune cells and chemical signals.
Autoimmune disease occurs when this balance breaks down. Triggers such as infections, genetic susceptibility, or environmental stressors can confuse the immune system. In some cases, pathogens resemble the body’s own tissues closely enough to cause mistaken attacks, a phenomenon known as molecular mimicry.
The immune system is not malicious—it is overzealous. It responds as if protecting the body, unaware that it has misidentified the enemy. This tragic misunderstanding can lead to chronic inflammation and tissue damage.
Understanding this mystery has transformed medicine, leading to treatments that calm immune activity rather than suppress it entirely, preserving protection while reducing harm.
4. Why Allergies Exist at All
Sneezing at pollen or reacting violently to peanuts seems absurd. Why would the immune system treat harmless substances as deadly threats? Allergies puzzled scientists for decades.
The explanation lies in the immune system’s ancient role in defending against parasites. Parasitic worms were once a major threat to human survival. The immune mechanisms that evolved to expel them—particularly those involving antibodies and inflammation—are extremely aggressive.
In modern environments, where parasites are far less common, this powerful machinery has fewer real targets. Instead, it sometimes misfires, reacting to pollen, dust, or food proteins as if they were parasitic invaders.
Allergies are not design flaws; they are evolutionary leftovers. The immune system is still wired for a world full of parasites, even though our lifestyles have changed dramatically.
This insight explains why allergies are more common in cleaner, urban environments and why early exposure to diverse microbes may reduce allergic risk.
5. Why Stress Makes You More Likely to Get Sick
The connection between stress and illness was once dismissed as psychological folklore. Today, it is a well-established biological reality.
When you experience stress, your body releases hormones such as cortisol and adrenaline. These chemicals prepare you for immediate survival, increasing heart rate and energy availability. However, they also suppress certain immune functions.
Short-term stress can actually enhance immune responses, sharpening alertness. But chronic stress tells the body to conserve resources. Over time, immune cells become less responsive, inflammation becomes dysregulated, and vulnerability to infection increases.
This explains why prolonged emotional strain, grief, or exhaustion often precedes illness. The immune system listens closely to the nervous system, adjusting its behavior based on perceived threat and safety.
The mystery here is not why stress affects immunity, but how deeply interconnected mind and body truly are.
6. Why the Immune System Causes Fever on Purpose
Fever feels like the body malfunctioning, yet it is one of the immune system’s oldest weapons. Raising body temperature creates a hostile environment for many pathogens, slowing their replication and weakening their structure.
At the same time, higher temperatures enhance immune cell activity, improving their ability to move, communicate, and destroy invaders. Fever is not a side effect of illness; it is an intentional strategy.
The immune system carefully regulates fever, balancing benefit against risk. Extremely high temperatures are dangerous, which is why the body rarely allows fever to rise beyond a narrow range.
Understanding fever as a controlled response rather than a malfunction has reshaped medical approaches, emphasizing moderation rather than automatic suppression.
7. How the Immune System Remembers Things You Forgot
You may forget your childhood home, but your immune system remembers the viruses you encountered there. Immune memory is remarkably durable, sometimes lasting a lifetime.
This memory is stored not in a single organ, but across populations of specialized cells distributed throughout the body. These cells persist quietly, occasionally dividing to maintain their numbers.
What makes this mysterious is that immune memory does not fade like neural memory. It does not require conscious recall or reinforcement. It is molecular, encoded in the structure of immune receptors and sustained through biological maintenance.
This form of memory is one of the most powerful survival tools humans possess. It allows the body to learn from experience and apply that knowledge automatically, silently protecting you long after you’ve forgotten the danger.
8. Why Some People Rarely Get Sick
We all know someone who seems immune to illness. While luck plays a role, the explanation is deeper.
Genetic diversity influences immune responsiveness. Certain gene variants make immune cells better at recognizing or responding to pathogens. Past exposure history also matters; people who encountered a wide range of microbes earlier in life may have more robust immune training.
Lifestyle factors—sleep, nutrition, physical activity, and stress—shape immune efficiency daily. The immune system is dynamic, responding continuously to internal and external signals.
This mystery reveals that immunity is not a fixed trait. It is a living system shaped by genetics, experience, and behavior, constantly adapting to the environment.
9. Why Inflammation Is Both Healing and Harmful
Inflammation is one of the immune system’s most misunderstood actions. It causes pain, swelling, and redness, yet it is essential for healing.
When tissue is damaged or infected, inflammation increases blood flow and immune cell access. This accelerates repair and defense. Without inflammation, wounds would not heal and infections would spread unchecked.
The mystery lies in chronic inflammation. When inflammatory responses fail to shut down, they damage healthy tissue and contribute to diseases such as arthritis, heart disease, and neurodegeneration.
Modern science has revealed that inflammation is not the enemy—it is imbalance. The immune system must know not only how to fight, but when to stop.
10. Why the Immune System Changes as You Age
As people age, their immune systems change in predictable yet puzzling ways. Older adults are more vulnerable to infection and respond less robustly to vaccines, yet they often experience more inflammation.
This phenomenon, known as immunosenescence, reflects the immune system’s long life of service. Over time, immune cells accumulate damage, memory becomes crowded with past experiences, and responsiveness declines.
At the same time, regulatory controls weaken, allowing low-level inflammation to persist. This contributes to age-related disease but also reflects the immune system’s attempt to maintain vigilance in a changing body.
Understanding this mystery has opened new paths for medicine, from improved vaccines to therapies aimed at restoring immune balance rather than simply boosting activity.
The Immune System as a Living Intelligence
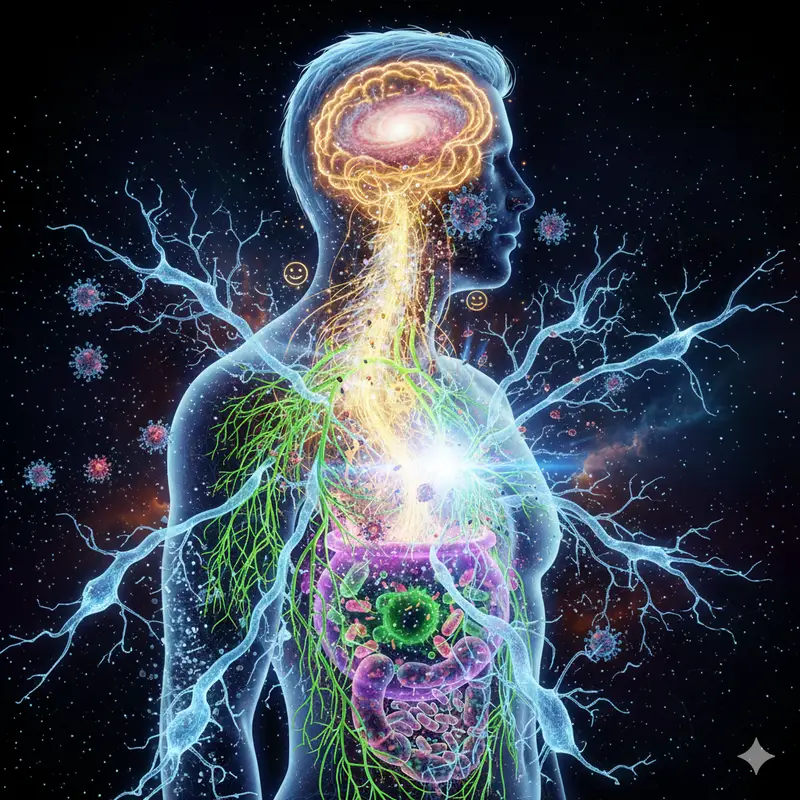
The human immune system is not just a defense mechanism. It is a learning system, a memory archive, and a dynamic network of communication. It senses danger, adapts to experience, and balances aggression with restraint.
What once seemed mysterious now reveals a deeper truth: the immune system is not separate from who we are. It reflects our past, responds to our present, and shapes our future.
Every fever, every allergy, every immune memory tells a story of survival. And as science continues to uncover its secrets, the immune system stands not as a cold machine, but as one of the most emotionally resonant systems in the human body—a silent guardian shaped by evolution, experience, and the fragile miracle of being alive.