Medicine is often portrayed as a precise science—a domain of white coats, stethoscopes, and solid answers. Yet even in the age of genome sequencing and robotic surgeries, there are cases that baffle doctors, scientists, and patients alike. These are the medical mysteries—puzzling illnesses, baffling symptoms, and elusive diagnoses that challenge the boundaries of human knowledge. They are the “X-Files” of hospitals, the real-life enigmas that push medicine into uncharted territory.
A medical mystery isn’t just about confusion or complexity; it’s about a situation that defies explanation, often for years or even decades. It might be a bizarre set of symptoms that doesn’t fit any known pattern. It might be a syndrome that appears in a single person or a community without any clear origin. Sometimes, it’s an illness that vanishes as inexplicably as it appeared, leaving behind only questions. In such cases, every test comes back normal, every hypothesis falls short, and the best minds in medicine are left scratching their heads.
These mysteries don’t just fascinate doctors—they grip the imagination of the public. They inspire documentaries, books, and endless speculation. But beyond the headlines, they also highlight something deeper about the human condition: how little we still know about the body, and how far we have yet to go in the quest to fully understand health and disease.
The Thin Line Between Diagnosis and Guesswork
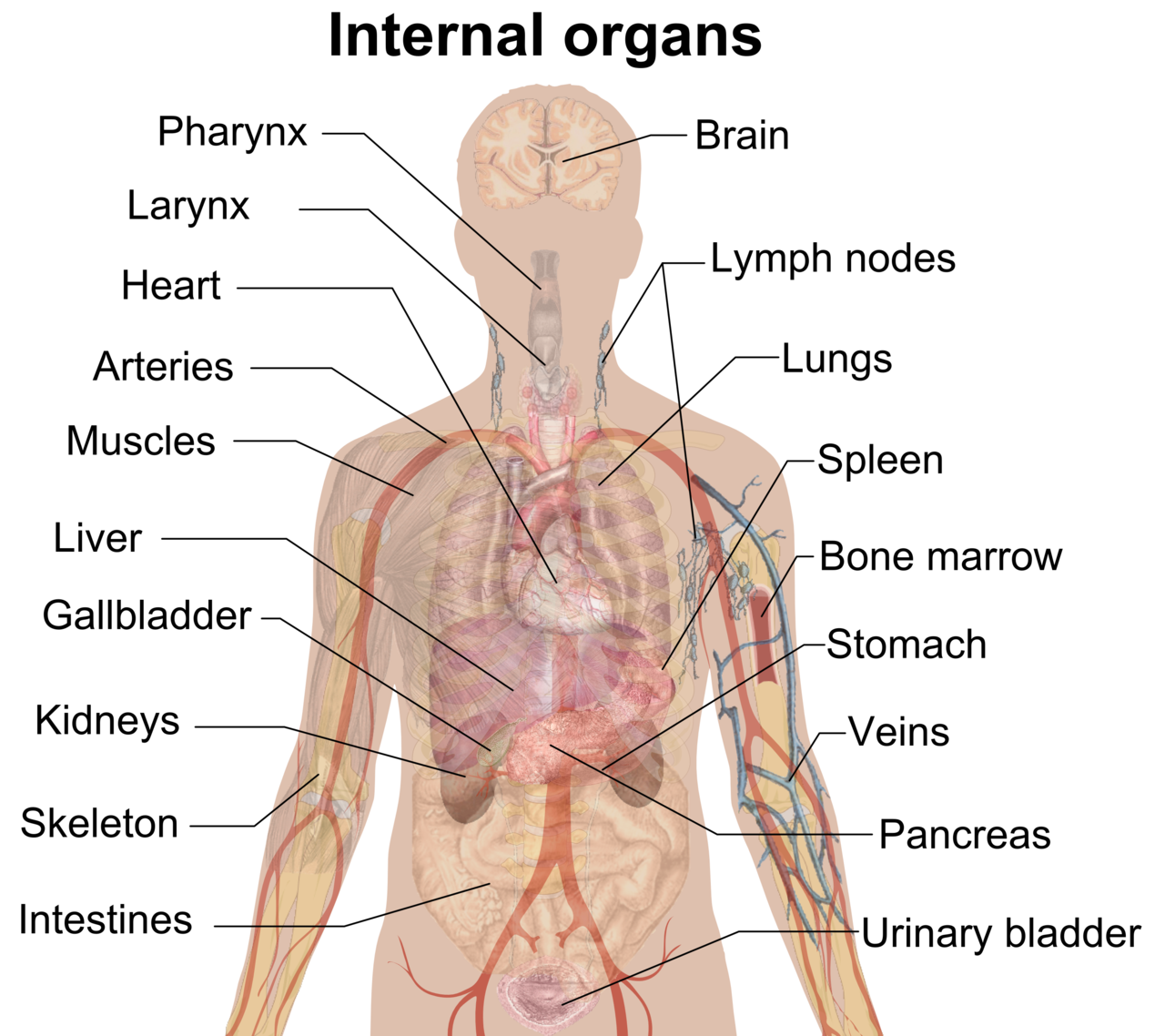
Modern medicine relies on the art of diagnosis, which is the act of naming a disease based on symptoms, lab results, and imaging. It’s a little like detective work—a combination of evidence, logic, and intuition. But even the most advanced diagnostic tools can be stymied by the sheer complexity of biology. The human body contains about 37 trillion cells, 60,000 miles of blood vessels, and a microbiome so complex it rivals a rainforest in biodiversity. It’s no surprise that sometimes, the systems go haywire in ways that no textbook has ever described.
Medical mysteries often start with a symptom that seems commonplace—chronic fatigue, fever, swelling, pain. What makes them mysterious is how these symptoms refuse to conform to any known disease model. Blood tests may show nothing wrong. Imaging might reveal anomalies without clear meaning. And when the usual suspects are ruled out, patients are often left in diagnostic limbo, sometimes for years.
This uncertainty can be harrowing. For the patients, it means living in a state of suspended animation—sick, but without a name for the sickness. For the doctors, it means confronting the limits of their knowledge. And for researchers, it becomes an opportunity—a puzzle that might lead to the discovery of a new disease, a new pathogen, or even a new mechanism of the body.
The Enigmatic Case of The Man Who Couldn’t Stop Sneezing
One of the most bizarre medical mysteries on record involved a young man from the UK named Christopher Sands. In 2006, Sands gained global attention for an ailment so peculiar it sounded like a joke—he sneezed, nonstop, every few seconds, for over two years. His uncontrollable sneezing fits began without warning, worsening day by day until they ruled his life. He couldn’t eat properly, hold a conversation, or sleep more than a few minutes at a time.
Doctors were dumbfounded. Allergies? No. Neurological disorder? Tests were inconclusive. Psychological origin? Unlikely. Specialists from across Europe evaluated him, and yet no one could pinpoint a cause.
Eventually, a chance discovery by an ear, nose, and throat specialist provided a clue. An MRI revealed a minor abnormality in Sands’ esophagus—a condition called gastroesophageal reflux disease (GERD). The acid reflux was believed to irritate nerves connected to the sinuses, triggering the sneezing. After surgery to correct the issue, the sneezing stopped. Case closed, maybe—but the mechanism remains speculative. It’s unclear why the condition presented with sneezing rather than more typical GERD symptoms. The mystery, in essence, remains.
The Girl Who Grew Old Before Her Time
Hutchinson-Gilford Progeria Syndrome is one of the rarest and most tragic conditions known to medicine. Affecting approximately one in four million newborns, this genetic disorder causes children to age rapidly—often appearing elderly by the age of ten. Wrinkled skin, joint stiffness, and cardiovascular disease emerge while the brain and intellect develop normally. Most children with progeria die from heart disease in their teens.
The most famous case is that of Hayley Okines, a British girl who became the face of progeria awareness. Despite her diagnosis, Hayley lived beyond her life expectancy and actively participated in medical trials. Her condition was traced to a mutation in the LMNA gene, which affects the structural integrity of the cell nucleus. But the mystery remains why this mutation leads specifically to premature aging. It doesn’t match any other aging process seen in normal human physiology. Nor does it answer why some cells seem to age rapidly while others do not.
Hayley’s life helped advance scientific understanding of progeria, and her participation in experimental treatments led to improved therapies. Yet the central mystery—how to stop or reverse this form of aging—remains unanswered.
The Dancing Plague of 1518
In July 1518, in the city of Strasbourg, a woman stepped into the street and began to dance. She danced for hours, then days. Soon, dozens of people joined her. Within a week, nearly 400 people were dancing uncontrollably in the streets. Some collapsed from exhaustion. Others reportedly died of heart attacks or strokes.
This strange event, now known as the Dancing Plague of 1518, is one of history’s most perplexing medical mysteries. It lasted for over a month, then vanished as mysteriously as it began. Historical accounts are surprisingly well-documented, yet the cause remains unknown.
Modern theories range from mass hysteria to ergot poisoning (a hallucinogenic mold that grows on rye). But none of the theories are definitive. Why did only certain people dance? Why didn’t everyone get sick? Why did it start and stop so suddenly? No pathogen was identified, and the psychological landscape of the time—marked by plague, famine, and religious fervor—may have played a role. But even today, no single explanation fully accounts for the phenomenon.
The Tragedy of The Girl Who Couldn’t Wake Up
In the late 2000s, a young girl named Annie from Texas began experiencing episodes where she would fall asleep for days, sometimes weeks, at a time. Her parents initially believed it was a strange form of narcolepsy. But this wasn’t ordinary sleep. Annie was unresponsive, barely moving, and would remain unconscious despite loud noise or physical stimulation.
Over time, her case grew more disturbing. Neurological tests, brain scans, and blood work revealed nothing abnormal. No epilepsy. No infections. No metabolic disorders. Doctors were stumped. A diagnosis of Kleine-Levin Syndrome was suggested, a rare condition also known as “Sleeping Beauty Syndrome,” characterized by episodes of hypersomnia, but even this did not fit perfectly.
Each episode left Annie weaker. Her education suffered. Her mental health declined. And her family remained in a state of constant fear. Cases like Annie’s underscore the helplessness that patients and families feel when there is no name for what’s happening. Despite consultations with top neurologists, no definitive cause was found, and treatment remained purely supportive. The sleeping spells eventually became less frequent, but the mystery endured.
When Your Body Thinks It’s Burning
Imagine feeling as though your skin is on fire every time you’re exposed to light—even artificial light from a screen or a light bulb. That’s the horrifying reality for people who suffer from a condition known as erythropoietic protoporphyria (EPP), a rare genetic disorder that leads to extreme photosensitivity. It’s been dubbed the “vampire disease” because patients must avoid sunlight entirely to prevent pain, swelling, and blisters.
For years, people with EPP were told it was “all in their head.” The symptoms didn’t always leave visible marks, and standard medical tests came back normal. It wasn’t until the 20th century that researchers identified the cause—an enzyme defect in the heme production pathway, leading to a buildup of toxic compounds in the skin that react violently to light.
Even with this knowledge, many mysteries remain. Why do symptoms vary so much between patients? Why do some cases worsen with age while others improve? Why do standard painkillers provide little relief during an episode? The disease is better understood today than a century ago, but for those living with it, it remains a daily—and painful—mystery.
The Man Who Couldn’t Stop Laughing
In the early 20th century, a man in Italy was brought to a clinic with an unusual complaint—he couldn’t stop laughing. This wasn’t joy or mirth; it was involuntary, mechanical, and distressing. His laughter would come in long, uncontrollable waves, often triggered by nothing at all.
Doctors eventually diagnosed him with a rare form of epilepsy known as gelastic seizures. These seizures originate from the hypothalamus, a deep part of the brain involved in emotion and hormone regulation. But why laughter? And why does this seizure differ so radically from more common types?
The case highlighted a deeper mystery about how the brain processes emotion. Laughter, like crying, is one of the most primal human responses, but it’s also among the least understood. While we now recognize gelastic seizures as a genuine neurological condition, many aspects remain unclear—including why some people with hypothalamic hamartomas (benign brain tumors) develop these seizures while others do not.
The Syndrome with No Name
Occasionally, a medical mystery remains so puzzling that it never even earns a name. Such was the case with a cluster of patients in New Brunswick, Canada, who in 2021 began reporting neurological symptoms including hallucinations, memory loss, weight loss, and muscle atrophy. Over 50 people were eventually affected, and rumors swirled of a new prion disease, environmental toxins, or even secret government experiments.
Health authorities conducted extensive investigations but failed to find a definitive cause. Tests for known prion diseases came back negative. No environmental toxins could be conclusively linked. Critics accused health officials of downplaying the crisis, while others claimed mass psychogenic illness was to blame. The case eventually faded from the news, unresolved and officially unexplained.
Such episodes highlight a painful truth: sometimes, medicine just doesn’t have the answers. Whether due to gaps in technology, limitations in funding, or the inherently elusive nature of biology, some mysteries are simply left unsolved.
What Medical Mysteries Teach Us
These strange, confounding, sometimes terrifying cases are not just curiosities for the medical community—they are invaluable windows into the limits and potential of modern science. Every mystery holds the potential to reveal something new. A single undiagnosed case can lead to the discovery of a novel disease. An unusual cluster might uncover a hidden toxin or a genetic variant never seen before.
Medical mysteries also serve as a humbling reminder of how little we truly understand. They challenge the hubris of certainty and force even the most seasoned doctors to think creatively. They invite collaboration across disciplines—from genetics to neurology, from psychiatry to immunology.
And perhaps most importantly, they humanize medicine. Behind every mystery is a person—a child who can’t wake up, a man who can’t stop sneezing, a woman who burns in the sunlight. These stories highlight not just the limits of science but the resilience of patients who live in those limits every day.
The Future of Solving the Unsolvable
With the rise of artificial intelligence, whole genome sequencing, and global data sharing, the future of medical mysteries may be one of rapid diagnosis and precise treatment. AI systems are already being trained to recognize rare diseases based on subtle symptom patterns. Genomic tools can uncover mutations that were invisible to past generations of doctors. Crowdsourced diagnostic platforms now connect patients with obscure conditions to specialists across the globe.
But even as the tools improve, the mysteries won’t disappear. Biology is dynamic, and new diseases are always emerging. Environmental changes, viral evolution, and even social behavior can create conditions for new syndromes to appear. The next pandemic might not be a virus but an autoimmune disorder that behaves like an infection, or a neurological condition triggered by environmental exposure.
Solving these puzzles will require not just technology, but compassion, curiosity, and a willingness to dwell in uncertainty. Medicine will always be, in part, an art.
Conclusion: The Enduring Fascination
What is a medical mystery? It is a story without an ending, a puzzle without a box, a question mark in the middle of a sentence. It is what keeps medicine alive—not just as a science, but as a journey. These cases capture the imagination, not just because they are strange, but because they represent the unknown frontier of human health.
In a world that often demands certainty and quick answers, medical mysteries teach patience. They remind us that every cure once began as a question, every diagnosis as a mystery. And for all the answers we have, it’s the unsolved that push us forward.
So the next time you hear about a case that “baffles doctors,” don’t dismiss it as sensationalism. Look closer. That may be the case that changes everything.