Pregnancy is one of the most transformative journeys in a woman’s life. It is a time when the body carries not only itself but also the beginnings of another life. For many women, pregnancy also overlaps with another kind of journey: travel. Whether for work, family obligations, or the irresistible pull of adventure, pregnant women often find themselves boarding planes, trains, or cars.
Traveling while pregnant is not only possible but can also be deeply enriching. It provides opportunities to bond with loved ones, enjoy restful vacations, or simply live life fully before welcoming a baby. Yet, it is also a journey that requires careful planning and mindful adjustments. The pregnant body is changing every week, and each trimester brings its own unique joys and challenges.
Traveling during pregnancy is not merely about logistics; it is about balancing safety, comfort, and the joy of exploration. Understanding how the body changes in each trimester—and how to travel safely during those phases—empowers women to move with confidence, grace, and peace of mind.
The First Trimester: Nurturing Beginnings on the Road
The first trimester, spanning weeks one through twelve, is a time of profound change hidden beneath the surface. While the baby is no larger than a plum by the end of this stage, the mother’s body is working tirelessly to create a nourishing environment. This is also when symptoms like morning sickness, fatigue, and heightened sensitivity make travel a little more complicated.
Navigating Nausea and Fatigue
Many women experience nausea and vomiting, often called “morning sickness,” though it can occur at any time of day. The triggers can be unpredictable—smells in an airport, motion during a car ride, or even certain foods. For this reason, it is wise to plan trips with flexibility. A pregnant traveler may need frequent breaks, light snacks on hand, or even to cancel activities if fatigue sets in.
Hydration becomes a quiet but powerful ally during the first trimester. Dehydration can worsen nausea and fatigue, so carrying a refillable water bottle is essential. Small, bland snacks like crackers or fruit can also keep blood sugar steady and minimize queasiness.
Considering Safety and Risk
The first trimester is when the risk of miscarriage is naturally higher, though travel itself does not cause miscarriage. Still, long flights, high-altitude destinations, or exposure to infections may pose risks that are worth discussing with a healthcare provider. For instance, areas with Zika virus should be avoided, as infections can harm the developing fetus.
Travel insurance that covers pregnancy-related issues can provide peace of mind during this delicate phase. It ensures that if unexpected medical care is needed abroad, the support will be available.
Choosing the Right Destinations
Shorter, slower-paced trips are often easier during the first trimester. Road trips with the flexibility to stop frequently, or calm retreats near home, may be more comfortable than long-haul flights. However, some women feel perfectly fine and enjoy adventurous travel even early on. Listening to the body is key—what feels nourishing and safe is different for everyone.
The Second Trimester: The Golden Window for Travel
The second trimester, from weeks thirteen through twenty-seven, is often described as the “sweet spot” of pregnancy. Many women find their energy returns, morning sickness fades, and the growing belly is not yet so large as to make movement uncomfortable. This trimester is often considered the best time for travel.
Embracing Comfort and Energy
With newfound energy, the second trimester offers opportunities for more ambitious travel. Many women take “babymoons”—special vacations taken before the arrival of the baby—during this stage. Whether lounging on a beach, exploring new cities, or hiking easy trails, travel can feel not only manageable but deeply enjoyable.
Still, comfort should be the guiding principle. Choosing accommodations with supportive beds, elevators, and nearby healthcare is practical. Packing maternity-friendly clothing that stretches with the body helps ensure ease throughout the trip.
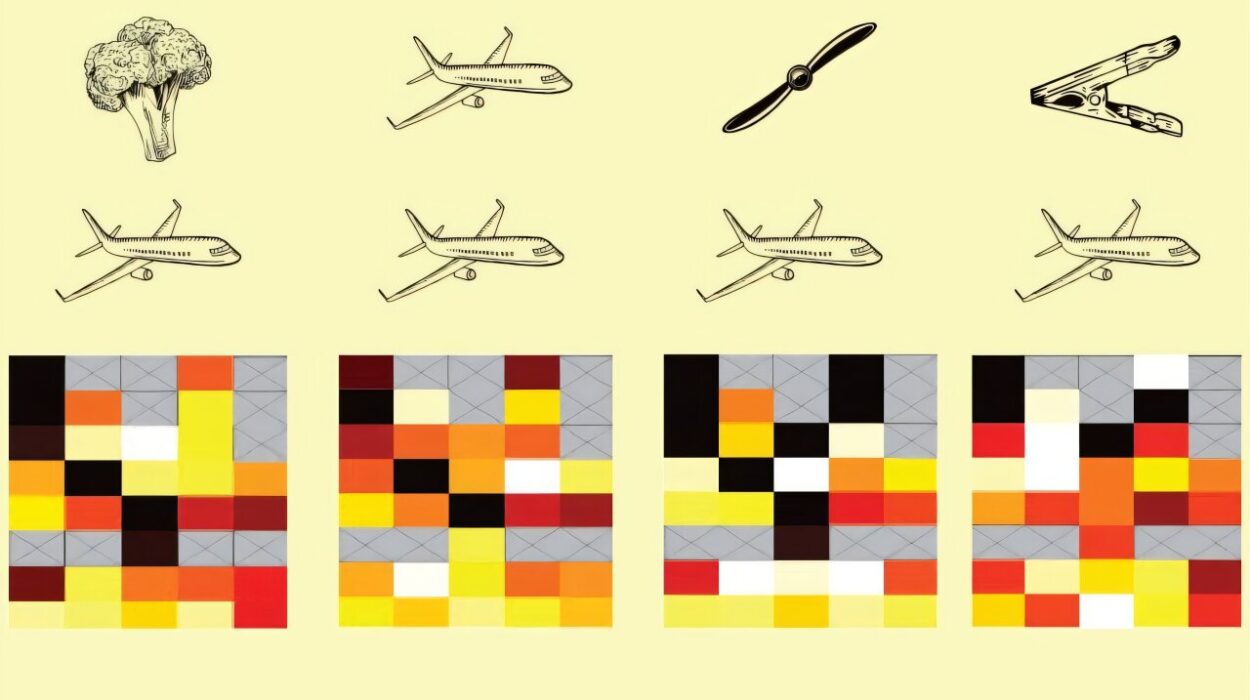
Air Travel During the Second Trimester
Airlines generally allow pregnant women to fly without restriction during the second trimester. It is, however, important to keep a few practices in mind. Walking around the cabin during long flights improves circulation and reduces the risk of blood clots. Compression socks can also help blood flow in the legs.
Window seats may seem cozy, but aisle seats are often better for easy bathroom access and freedom to stretch. Carrying prenatal vitamins, medical documents, and snacks ensures stability even in unpredictable travel conditions.
Safety Considerations Abroad
Vaccinations and preventive health measures may be necessary depending on the destination. Pregnant women should avoid certain live vaccines, so medical guidance before international travel is crucial. Mosquito-borne illnesses like malaria or dengue also pose serious risks during pregnancy, making destination research vital.
Adventures with Care
The second trimester allows for exploration, but with limits. Activities that involve extreme exertion, altitude above 10,000 feet, or high risk of falling should generally be avoided. That means no scuba diving, no mountain climbing at extreme heights, and caution with amusement park rides. But gentle adventures—walking tours, swimming, nature trails—are not only safe but invigorating.
The Third Trimester: Preparing for the Final Stretch
The third trimester, spanning weeks twenty-eight through forty, is the most physically demanding stage of pregnancy. The body is preparing for birth, the belly is at its fullest, and fatigue often returns. Travel during this time is possible, but it requires heightened caution and realistic expectations.
Navigating Physical Challenges
Sitting for long periods, whether in a car or on a plane, becomes more difficult as the belly expands. Swelling in the feet and ankles is common, and frequent restroom breaks are a necessity. Pregnant travelers in this trimester benefit from building in extra time for rest, stretching, and bathroom stops.
The risk of preterm labor increases in the third trimester. While most women do not deliver until after thirty-seven weeks, the unpredictability of labor makes traveling far from healthcare facilities riskier. For this reason, many airlines restrict travel after week thirty-six, and some even earlier for international flights.
Travel Close to Home
In the final trimester, local or regional trips are often more practical than international travel. Weekend getaways within driving distance or restful stays close to a trusted hospital provide the joy of travel without unnecessary risk.
Car travel may be more manageable, especially when breaks can be taken as needed. Using a seatbelt properly—lap belt under the belly and across the hips, with the shoulder strap between the breasts—provides both comfort and safety.
Emotional Considerations
The final weeks of pregnancy carry a mixture of anticipation, anxiety, and excitement. Travel during this time should nurture, not exhaust. Choosing destinations that are calming, supportive, and low-stress is essential. A mountain cabin, a quiet seaside town, or a spa retreat can provide restorative energy before the arrival of the baby.
General Safety Principles for Traveling While Pregnant
Listening to the Body
One universal rule for pregnant travel is listening to the body’s signals. Pregnancy transforms how energy is used, how digestion works, and how balance is maintained. Ignoring cues of fatigue, hunger, or discomfort can make travel harder. Respecting those cues allows for smoother journeys.
Communication with Healthcare Providers
No travel plan should be made without consulting a healthcare provider. Each pregnancy is unique, and what is safe for one woman may not be advisable for another. Conditions such as high blood pressure, risk of preterm labor, or placenta previa may limit travel. Having medical clearance provides confidence and clarity.
Access to Healthcare on the Road
Researching healthcare facilities near the destination can be a lifesaver. Keeping copies of prenatal records, blood type, and doctor’s contacts ensures that if medical care is needed, it is accessible. Many women also carry travel insurance that specifically covers pregnancy-related emergencies.
Nutrition and Hydration
Pregnancy increases nutritional needs. Traveling with healthy snacks—nuts, fruit, yogurt—can prevent energy dips. Staying hydrated is especially important, particularly in hot climates or on long flights where dehydration is common.
Emotional Well-being
Travel during pregnancy is not only about physical safety but also about emotional well-being. Stress, anxiety, or overexertion can take a toll on both mother and baby. Building trips around rest, joy, and connection helps make travel a nourishing experience.
Traveling with Love and Intention
Every pregnancy is a story, and travel becomes a chapter within it. For some women, it is a quiet chapter, marked by gentle getaways. For others, it is adventurous, filled with journeys to new places. Whatever the form, traveling while pregnant is more than movement through space—it is movement through a unique moment in life.
Safety and comfort must remain the guiding stars, but within those boundaries lies the freedom to explore, connect, and savor. The laughter shared with a partner on a babymoon, the calm of watching the sunset from a beach, or even the small joy of sipping tea in a new city can become treasured memories before the whirlwind of parenthood begins.
Pregnancy does not close the door to adventure. Instead, it transforms it. It asks women to move with greater awareness, to balance the needs of two lives, and to approach travel not with recklessness but with reverence. With thoughtful planning, medical guidance, and compassionate self-care, the world remains open—even as life within the womb is just beginning.