Endometriosis is not just a condition; it is a quiet epidemic that steals years from the lives of women and girls. It hides in the shadows of pain, dismissed too often as “just bad cramps” or “normal period discomfort.” But for the nearly 200 million people worldwide who live with this chronic disease, the truth is far more agonizing.
In endometriosis, tissue similar to the lining of the uterus grows outside the uterus. These rogue cells, behaving as if they still belonged inside the womb, respond to hormonal cycles just like the uterine lining—thickening, breaking down, and bleeding. But unlike menstrual blood that exits the body, this blood has nowhere to go. It causes inflammation, scarring, severe pelvic pain, and in many cases, infertility. Some wake up each day to pain so intense it feels like their body is tearing itself apart from the inside. Others suffer in silence, their symptoms minimized or misunderstood for years, even by medical professionals.
Despite how common and debilitating endometriosis is, there remains a startling absence of effective, non-invasive diagnostic tools. A patient might spend a decade or more enduring symptoms before receiving a correct diagnosis. In a time when we can sequence the human genome in a day and send spacecraft to Mars, the absence of a simple diagnostic test for such a widespread disease is not just a scientific failure—it is a societal one.
A Missed Opportunity in Plain Sight
In most clinical settings, the investigation into possible endometriosis begins with blood tests, imaging scans, invasive pelvic exams, and often ends with laparoscopic surgery to confirm diagnosis. But what if the answer has been right in front of us—or more accurately, within us—all along?
Each month, millions of people menstruate, shedding blood and tissue from the uterus. And yet, this biological material, rich with cellular and molecular information, is typically dismissed as waste. It is flushed, discarded, and stigmatized. Menstrual blood is a diagnostic goldmine hiding in plain sight, overlooked not because of science, but because of centuries-old taboos.
Professor Dipanjan Pan, a nanomedicine expert at Penn State University, saw the potential others ignored. Rather than accepting the limitations of conventional testing, he asked a simple but revolutionary question: what if menstrual blood could tell us who has endometriosis—quickly, accurately, and painlessly?
What followed was a breakthrough that could transform women’s health care forever.
Nanoscience Meets Menstrual Blood
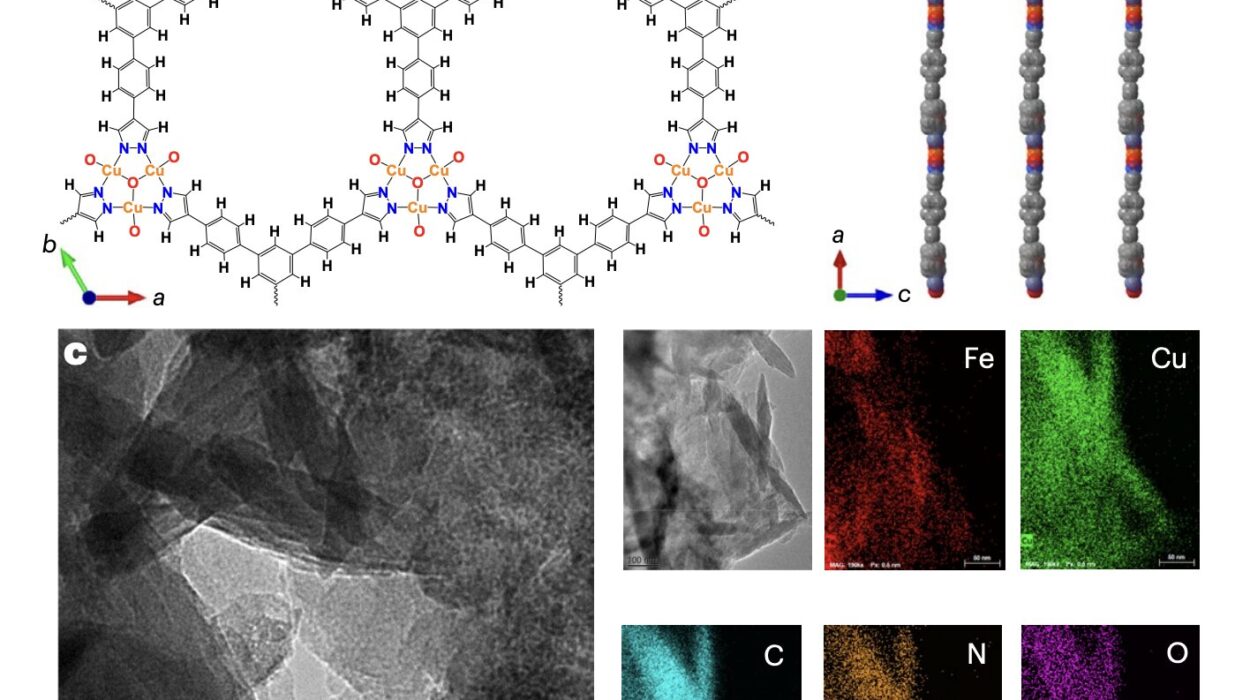
To unlock the diagnostic secrets hidden in menstrual blood, Pan and his research team turned to one of the most cutting-edge materials in modern science: borophene. This ultra-thin, two-dimensional material is a derivative of boron, known for its exceptional sensitivity and versatility. Similar to graphene—which revolutionized electronics—borophene is now being hailed as a new frontier in biomedicine.
What makes borophene truly remarkable isn’t just its electrical properties or thinness, but its biocompatibility. It can safely interact with the human body and degrade harmlessly, a critical feature for any material involved in health monitoring. But unlike graphene, borophene has remained more elusive in laboratories due to the complexity of its synthesis—until now.
Traditional synthesis methods use alcohol-based solvents, which can degrade the material or introduce harmful residues, making it unfit for biomedical use. Pan’s team devised a safer, more efficient method. They used water instead of harsh solvents to create pristine borophene nanosheets by dispersing powdered boron into water and carefully reconstructing its molecular architecture. This novel approach allowed them to create a clean, high-quality substrate for further modification.
But the nanosheets were only the beginning. To transform them into a diagnostic tool, the researchers needed them to recognize a specific protein—HMGB1.
The Signature of a Disease
HMGB1 is not just any protein. It plays a significant role in inflammation and immune system signaling and has been implicated in the progression of endometriosis. Patients with the disease often exhibit elevated levels of HMGB1 in their menstrual blood, even in early stages when symptoms may still be mild or ambiguous. This makes it a powerful biomarker for early detection—if it can be reliably identified.
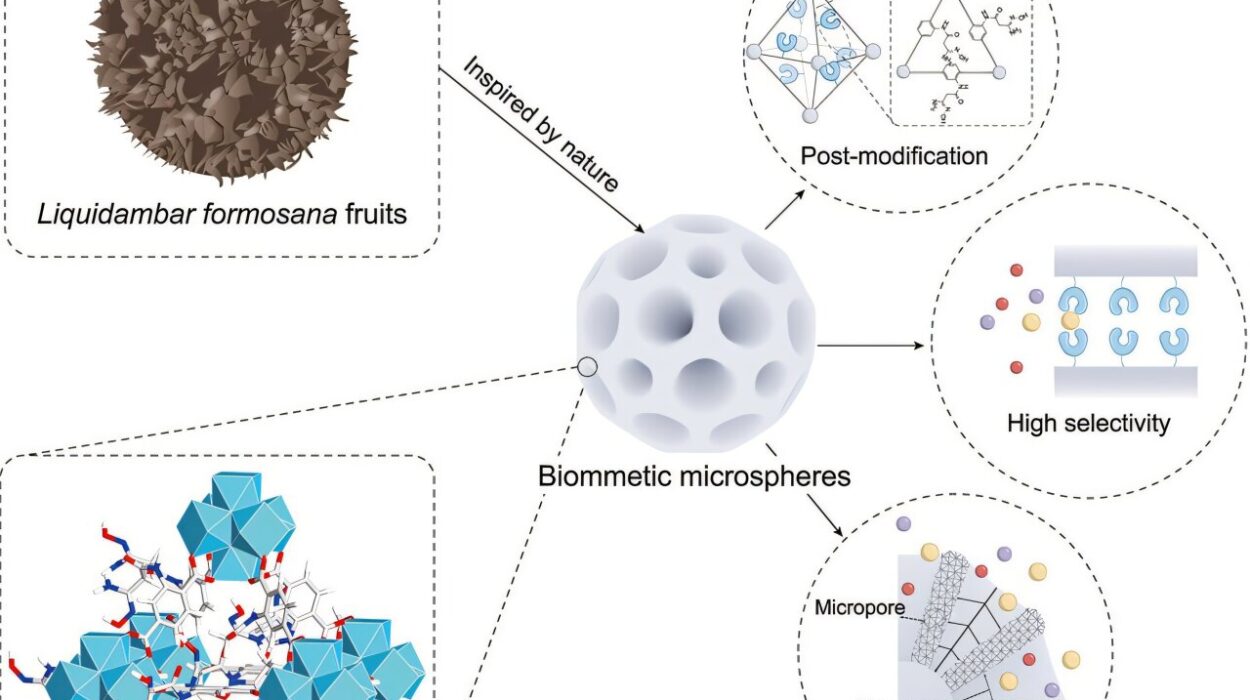
Pan’s team engineered the borophene nanosheets to become sensitive detectors by binding them with antibodies specifically designed to latch onto HMGB1. The process was likened by Pan to planting a garden: the nanosheets had to be smooth and clean, like fertile soil, before the antibodies could be “planted.” Once established, these antibodies would function like vigilant sentries, capturing any HMGB1 proteins present in a sample.
With the antibodies firmly anchored, the nanosheets were integrated into a prototype diagnostic device—one that looks and functions much like a common pregnancy test. A drop of menstrual blood flows across the strip. If HMGB1 is present, it binds with the antibodies, darkening the test area and producing an unmistakable visual cue.
Five Times the Sensitivity, a Thousand Times the Possibility
When tested, the prototype did more than just detect HMGB1—it did so with unprecedented sensitivity. The device was found to be 500% more sensitive than existing laboratory techniques, successfully identifying HMGB1 even in low concentrations that might appear in the early stages of endometriosis.
This breakthrough is more than a technical achievement; it is a shift in what we believe is possible in diagnostics. Existing methods not only require specialized labs and equipment but also depend heavily on patient history and symptomatic reporting, which can be highly variable. Worse still, invasive surgery remains the gold standard for diagnosis. Pan’s device offers a radically different path—one where detection is non-invasive, discreet, and immediate.
It is not difficult to imagine what this could mean for someone living in a rural community far from advanced medical centers, or for a teenager just beginning to experience unexplained menstrual pain. With a test like this, early detection becomes accessible. Treatment can begin before the disease causes irreversible damage. Lives can be changed.
Beyond the Lab: From Pads to Possibility
Perhaps one of the most exciting prospects lies in the future direction of the research. Pan envisions integrating this diagnostic technology directly into menstrual products—pads or tampons that silently monitor HMGB1 levels with every cycle. The data could be sent to a smartphone or device, enabling real-time health tracking without the need for a clinic or even a conversation. Such an innovation would not only bring diagnosis into the home, but also destigmatize menstruation by highlighting its value in medical science.
In regions where access to health care is limited or where cultural stigma prevents open discussion about reproductive health, this kind of wearable diagnostic could offer an unprecedented lifeline. It empowers the individual, putting the power of detection literally into their hands.
The implications don’t stop at endometriosis. The same borophene-based technology could be adapted to detect a wide range of biomarkers—from HPV to cervical cancer to infectious diseases. What Pan and his team have built is not just a test, but a platform for future medical innovation.
Fighting Stigma with Science
Underneath the science lies a deeper truth: menstrual blood, long regarded as unclean, wasteful, or taboo, is finally being recognized for what it is—a biological resource rich with diagnostic potential. By creating a test that centers menstruation rather than shames it, Pan and his team are not just changing the conversation around endometriosis. They are helping to reclaim the narrative around female health.
Social stigma has delayed scientific progress for far too long. Cultural taboos have prevented meaningful research into menstruation, pain, and the diseases that disproportionately affect people assigned female at birth. It is not merely a lack of knowledge that has slowed innovation, but a lack of will. Pan’s work challenges that inertia, shining a light into the darker corners of medical neglect.
Toward a Future Without Delay
Endometriosis takes an average of seven to twelve years to diagnose in many parts of the world. That is seven to twelve years of pain, confusion, and damage. Seven to twelve years of missed opportunities to intervene, to treat, to heal.
Imagine a future where diagnosis takes minutes instead of years. Where a young girl experiencing her first painful periods receives an answer instead of silence. Where no one has to suffer in doubt, waiting for a doctor to finally listen.
That future is no longer science fiction. It is being built today in research labs like Pan’s—with borophene, with vision, and with a fierce belief in the value of every life.
The Promise of a New Era
In the end, science is not just about discovery. It is about dignity. It is about saying to those who have suffered unseen and unheard: we see you, we believe you, and we are working for you.
The work of Professor Dipanjan Pan and his colleagues represents more than a technological leap. It is a symbol of what happens when science refuses to look away—when it chooses empathy over indifference and listens to the voices long silenced by shame.
With every nanosheet of borophene, with every HMGB1 protein captured, we move closer to a world where pain is not normalized, where periods are not dismissed, and where endometriosis is not a life sentence, but a solvable puzzle.
Because sometimes, the answers we need are not hidden in the stars or buried in the genome—they are already flowing through us, waiting for someone to finally pay attention.
Reference: Satheesh Natarajan et al, Photoinduced Immobilization on Two-Dimensional Nano Borophene Spatially Orients Capture Antibody for Highly Sensitive Biological Interactions, ACS Central Science (2025). DOI: 10.1021/acscentsci.5c00474