In the labyrinth of the human brain—an organ both delicate and unyielding—an unexpected guardian may be emerging from the shadows. These guardians are not neurons, not blood vessels, not even the specialized glial cells once thought to be mere support structures. They are microglia, the brain’s resident immune cells, once dismissed as passive janitors of neural debris.
But now, a groundbreaking study from the University of Virginia School of Medicine is rewriting the story. These tiny cells, it turns out, may have a hand on the throttle of something far more essential than previously imagined: the very flow of blood that nourishes the mind.
The implications are profound. Microglia, researchers now suggest, are not only defenders against infection and clean-up crews for dead cells. They are regulators of capillary tone—fine-tuners of the narrowest vessels that feed the brain. And in diseases like Alzheimer’s, where memory fades and cognition fractures, that regulation may be going terribly awry.
Blood, Brains, and an Unsuspecting Culprit
Every thought, every memory, every heartbeat that echoes within your awareness is made possible by blood. The brain, despite its relatively small size—just 2% of your body’s mass—demands a staggering 20% of your energy. To keep up, it’s wrapped in an intricate network of more than 400 miles of blood vessels, branching into the finest of capillaries that reach every neuron like roots drawing nourishment from rich soil.
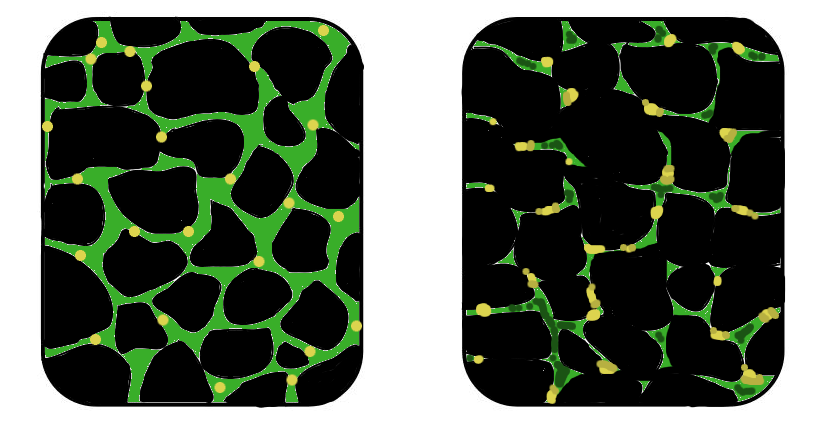
But what if the tiniest of these blood highways began to narrow? What if the nutrients they were meant to deliver began to slow, or stall altogether?
That’s what happens in neurodegenerative diseases. In Alzheimer’s, vascular dementia, and even some forms of Parkinson’s, the brain’s capillaries begin to misbehave. And scientists have long known that myeloid cells—immune cells related to microglia—could be involved. What they didn’t know, until now, was how microglia themselves might be regulating that blood flow.
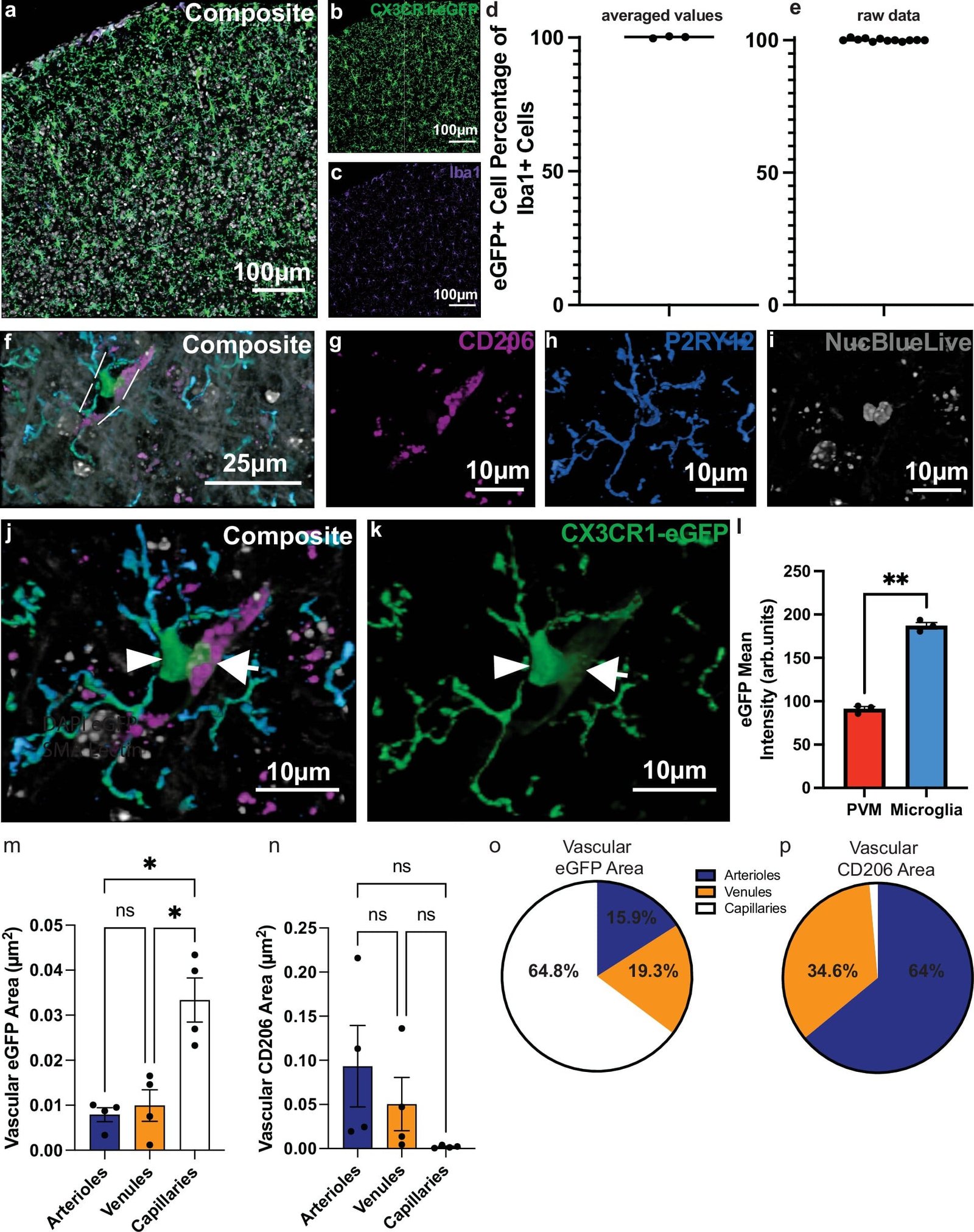
The new study, published in Nature Communications, is led by Dr. Ukpong B. Eyo, a neuroscientist at UVA’s Center for Brain Immunology and Glia (BIG Center) and the UVA Brain Institute. Together with first author Dr. William A. Mills III and their team, Eyo has identified microglia as direct influencers of capillary function. When these cells are removed, capillaries narrow and their ability to deliver blood diminishes. Restore the microglia, and normal blood flow returns.
The Enzyme in the Spotlight
Beneath this discovery lies a biochemical mystery unraveling before our eyes. The team identified a specific enzyme within microglia that appears to control their influence over blood vessel tone. Though this enzyme has been targeted before in Alzheimer’s research—often with underwhelming results—this study suggests a crucial difference: timing.
The therapeutic window during which microglia can most effectively regulate blood flow may be fleeting. “Our study suggests that these therapeutics would have maximal benefit if prescribed according to the therapeutic window of microglia in Alzheimer’s,” Mills explains. In other words, interventions might fail not because the science is flawed, but because the therapy came too late.
It’s a tantalizing prospect. If scientists can pinpoint when and how to engage this enzyme—before the capillaries begin to fail—then blood flow to the brain might be preserved or even rejuvenated. That means clearer thinking, preserved memory, and possibly a future where cognitive decline can be slowed or reversed.
Beyond Protection: A New Role for Microglia
For decades, microglia have been viewed through the lens of pathology. They became active when something went wrong—infection, inflammation, injury. But now, they are being seen not only as responders but as regulators, even guardians of cerebral function.
Microglia, the study found, regulate basal capillary tone—the natural state of constriction or relaxation in the tiniest vessels. This tone determines how freely blood can pass through, how effectively oxygen and nutrients reach every neuron. All microglia seem to participate in this regulation, not just a specialized few. That universality elevates their importance.
Their absence, however, is striking. Remove them, and capillaries tighten like arteries in cold air. Blood slows, the brain begins to starve—not in a dramatic collapse, but in a slow, creeping suffocation. It is a biological silence that mimics the slow fade of memory itself.
Alzheimer’s and the Quiet Crisis of Flow
Alzheimer’s disease is often described as a disease of plaques and tangles—amyloid and tau proteins building up in the brain until cognition unravels. But there’s another crisis unfolding, one that occurs quietly in the spaces between those hallmark lesions: the failure of blood to arrive where it’s needed most.
This vascular dysfunction has long been suspected to contribute to Alzheimer’s symptoms, even exacerbating the accumulation of harmful proteins. Starved neurons don’t just underperform—they begin to die. With this new research, scientists now have a clearer view of one possible culprit: microglia that have lost their way.
In Alzheimer’s, microglia are known to become dysregulated. They can become hyperactive, attacking healthy tissue, or they can retreat into dormancy. In either state, their ability to regulate blood flow may falter. That failure may be one of the earliest changes in the disease process—an invisible thread unraveling years before symptoms appear.
By restoring healthy microglial function, it may be possible to stabilize blood flow early on, creating a more favorable environment for neurons to survive and thrive. It’s not just about clearing plaques anymore—it’s about feeding the brain.
Unlocking the Future: Questions That Could Change Everything
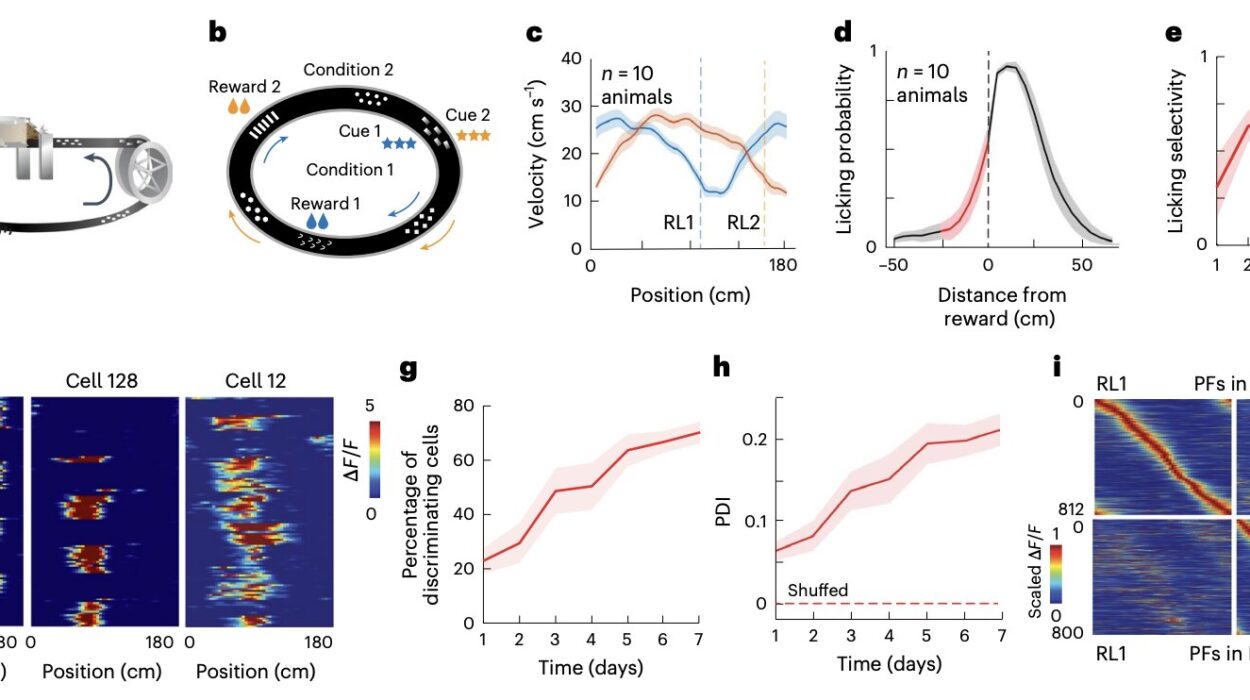
The research opens more doors than it closes, raising urgent and exciting questions. When, exactly, do microglia begin their role in capillary regulation? Is it present from birth, or does it develop later? Do these immune cells work alone, or in tandem with neurons, astrocytes, and endothelial cells? In diseases of development—like autism spectrum disorder—could microglial dysfunction contribute through compromised blood flow?
Dr. Eyo and his team are pursuing these mysteries with renewed focus. They are especially intrigued by the idea of microglial replacement. Could transplanting healthy microglia into a diseased brain restore proper blood flow? Could we develop therapies that guide dysfunctional microglia back to health without the need for drugs that flood the whole brain with imprecise chemicals?
The possibility of “microglial medicine” is on the horizon. These cells are everywhere in the brain, uniquely positioned to monitor, respond, and now—perhaps—heal. The idea that they could be fine-tuned to improve the most basic function of brain life—its nourishment—could shift the trajectory of not only Alzheimer’s but other forms of dementia, stroke recovery, and traumatic brain injury.
A New Vision of the Brain’s Immune Intelligence
There’s something poetic in the idea that immune cells—so often agents of destruction—might also be architects of life. Microglia are part of the brain’s quiet intelligence, an immune system adapted not just for defense, but for balance, communication, and now, delivery.
They listen to chemical signals, interpret electrical rhythms, and adjust the literal flow of life through the brain’s intricate web. Like sentinels at every junction, they ensure that each thought, each spark of memory, is backed by energy.
In the end, this study doesn’t just redefine our understanding of microglia—it reframes the nature of brain health itself. No longer is cognition the exclusive domain of neurons. It is a collective act, sustained by glia, blood vessels, enzymes, and a symphony of cells working in concert.
Toward a Future Without Forgetting
If science continues down this path, the future of Alzheimer’s treatment may look radically different. Instead of attacking plaques or suppressing inflammation, we may focus on restoring balance—reawakening the silent stewards of capillary health.
Through microglia, we might one day ensure that the aging brain remains nourished, alert, and alive. That memories are not swallowed by silence. That names and faces do not vanish into fog. That the spark of self can burn just a little longer, even in the twilight.
Reference: William A. Mills et al, Microglial cyclooxygenase-1 modulates cerebral capillary basal tone in vivo in mice, Nature Communications (2025). DOI: 10.1038/s41467-025-60753-x