An eye-opening analysis of more than 4 million South Koreans has revealed a startling correlation between body weight and the risk of suicide. According to research published in BMC Psychiatry, underweight individuals are 44% more likely to die by suicide compared to their normal-weight peers. In contrast, those who are overweight or obese show a 20–30% lower risk of suicide than individuals in the normal weight range.
This discovery, based on a massive dataset from South Korea’s National Health Information Database (NHID), is more than just another set of numbers. It highlights a paradox that challenges prevailing cultural assumptions about body image and mental health. In a society grappling with rising suicide rates and an escalating obesity crisis, this study raises vital questions: Why are underweight individuals at such high risk? And could carrying extra weight actually provide a protective buffer against suicidal behavior?
Suicide: A Complex and Devastating Reality
Suicide is far more than a personal tragedy; it is a pressing global public health crisis. The act of intentionally ending one’s own life often stems from a multifaceted tangle of mental, social, emotional, and biological factors. Globally, suicide ranks among the leading causes of death, particularly among adolescents, older adults, and socially marginalized individuals.
The ripple effect of a suicide extends well beyond the individual. Families are shattered, friends are left grappling with guilt and grief, and communities suffer long-term psychological and social consequences. It’s an epidemic of silence, stigma, and suffering.
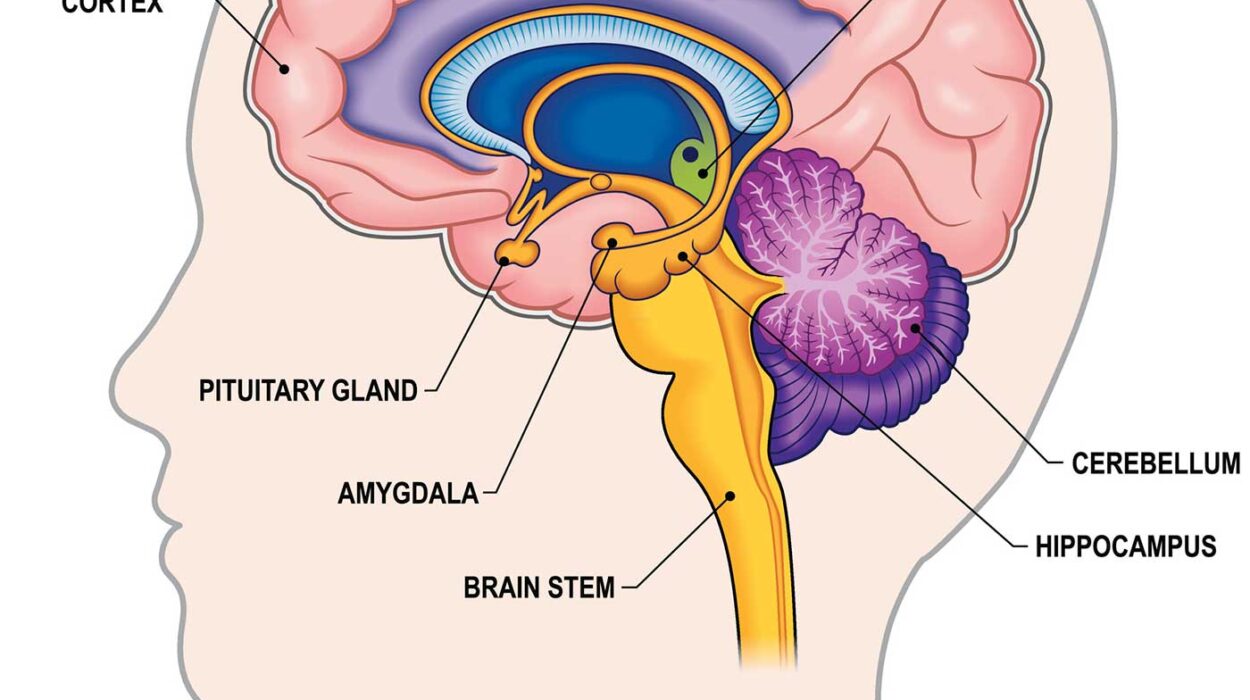
Over decades, research has uncovered a vast array of suicide risk factors—from neurochemical imbalances and chronic illnesses to trauma, social isolation, and financial hardship. Among the better-known biological contributors are specific genetic variations that affect serotonin signaling in the brain—a key player in mood regulation and impulse control.
But this new study introduces an additional, less expected variable: body mass index (BMI).
The Korean Study: A Nationwide Investigation
Dr. Joonyub Lee and his colleagues undertook a remarkable investigation to examine the relationship between BMI and suicide risk. Their research was motivated by two disturbing national trends: South Korea’s alarmingly high suicide rate—one of the highest among OECD countries—and a rapid increase in obesity.
To understand how body weight might influence suicide risk, the team analyzed data from the NHID, a comprehensive resource that includes national health screenings, insurance claims, diagnostic histories, and lifestyle factors. The study involved a staggering 4,045,081 adults, all over the age of 19, who had undergone health screenings in 2009. These individuals were tracked over the next 12 years, until death by suicide or the end of the study period in 2021.
Using a multifactorial approach, the researchers incorporated not only BMI and waist circumference (as a measure of abdominal obesity) but also co-occurring diagnoses such as depression, anxiety disorders, schizophrenia, and eating disorders. Additional variables included household income, alcohol consumption, blood glucose levels, and even serotonin levels.
The Results: An Unexpected Protective Effect of Higher Weight
The findings revealed a clear and consistent pattern: suicide risk declined as BMI increased.
- Underweight individuals faced a 44% higher risk of suicide compared to those in the normal BMI range.
- Overweight individuals showed a 21% reduced risk.
- Obese individuals demonstrated a 29% lower risk.
These results remained statistically significant even after controlling for critical confounding factors—such as diagnosed major depressive disorder (MDD) and living arrangements (i.e., whether or not someone lived alone).
This phenomenon, known as the “obesity paradox,” has been observed in other areas of medicine, where higher BMI is unexpectedly associated with lower mortality rates, particularly in older populations or individuals with chronic diseases. The Korean study adds a new dimension to this paradox by suggesting that a higher BMI may also buffer against suicide.
Interpreting the Findings: What’s Going On?
The results raise profound questions about the biological and psychosocial interplay between body weight and suicidal behavior. Why might underweight individuals be at higher risk, and why would a higher BMI offer protection?
Several hypotheses emerge:
1. Physiological Resilience and Energy Stores
Low body weight often reflects poor nutritional status, chronic illness, or underlying mental health conditions such as anorexia or chronic depression. Being underweight can deplete energy stores—both physically and emotionally—leaving individuals more vulnerable to hopelessness, fatigue, and despair.
By contrast, higher fat and energy reserves may offer metabolic and neurochemical stability, possibly influencing neurotransmitters like serotonin and dopamine, which are critical to mood regulation.
2. Social Stigma and Body Image
In many East Asian societies, particularly South Korea, there is an intense cultural emphasis on thinness. Individuals who fail to meet these ideals—especially young women and adolescents—may experience shame, self-criticism, or social alienation. However, those who are already underweight might paradoxically internalize harsher standards, leading to increased psychological distress.
Obese individuals, though also subject to stigma, may have developed coping mechanisms or received greater support for mental health interventions due to the visibility of their condition.
3. Hormonal and Inflammatory Factors
Fat tissue is more than passive storage—it is an active endocrine organ. It secretes hormones like leptin and adiponectin, and cytokines that influence inflammation, mood, and stress response. Some scientists speculate that a certain level of systemic inflammation or metabolic activity associated with obesity might influence neuropsychiatric stability—though this remains a subject of debate.
4. Chronic Illness vs. Psychiatric Burden
Underweight individuals often suffer from chronic or untreated mental health conditions like eating disorders, anxiety, or depression, all of which are strongly correlated with suicide risk. Conversely, some overweight and obese individuals may receive more frequent medical monitoring, improving the chance of detecting and treating psychiatric symptoms early.
Implications for Mental Health and Public Policy
This study opens up a new frontier in public health policy and suicide prevention strategies. It underscores the importance of screening for suicide risk in underweight individuals, who may be overlooked in traditional mental health assessments. Doctors and mental health professionals might need to adopt more nuanced approaches, integrating BMI and physical health data into psychiatric evaluations.
It also prompts policymakers to reconsider the messaging around body weight. Public health campaigns that focus exclusively on the dangers of obesity may inadvertently neglect the risks faced by underweight individuals—who are often perceived, wrongly, as healthier or more disciplined.
Furthermore, this research supports a biopsychosocial model of suicide risk—one that incorporates biological, psychological, and social dimensions in understanding and addressing suicidal behavior.
Cultural Considerations: Why Context Matters
It is critical to note that this study was conducted in South Korea, a nation with unique cultural attitudes toward body image, success, and social status. The societal pressure to conform to aesthetic ideals is exceptionally intense, particularly for young people navigating education and employment.
Moreover, suicide in South Korea remains a major public health issue. The nation has implemented several nationwide campaigns and legislative measures, including media guidelines and mental health reforms, but the numbers remain high.
Thus, while the findings offer crucial insights, they may not universally apply across different countries and cultures. In Western societies, for instance, where obesity carries different social meanings and comorbidities, the relationship between BMI and suicide may be shaped by a different set of factors.
Future Directions: What We Still Don’t Know
Despite its large sample size and long follow-up period, the study leaves important questions unanswered. For one, the data is observational—it shows correlation, not causation. We cannot say with certainty that being underweight causes higher suicide risk, only that the two are statistically linked.
Additionally, the mechanisms behind the observed associations remain unclear. More research is needed to explore:
- The neurobiological changes linked to low or high BMI.
- How social support varies across weight categories.
- The role of cultural perception in internalized distress.
Randomized interventions or longitudinal mental health studies that integrate biological, behavioral, and environmental data could provide deeper insights into these complex dynamics.
Conclusion: A Weighty Matter for Mental Health
The Korean study offers a powerful reminder that mental health is inseparable from physical health. Our bodies are not merely vessels for our minds—they are active participants in shaping our emotions, behaviors, and ultimately, our will to live.
By illuminating the link between BMI and suicide, this research invites us to rethink our assumptions—about weight, wellness, and what it means to support someone in distress. It also reminds clinicians and caregivers to look beyond appearances and consider the hidden struggles behind underweight frames.
In a world increasingly fixated on outward perfection, this study serves as a call to focus inward, on empathy, understanding, and a more holistic view of human well-being. Because sometimes, what we see on the outside doesn’t reflect the turmoil within—and in that silence, lives are lost.