Cancer is one of humanity’s most relentless adversaries. It is not a single disease but a constellation of over a hundred different conditions, each characterized by the uncontrolled growth and spread of abnormal cells. Despite decades of medical progress, cancer still claims millions of lives every year. For patients and their families, the diagnosis often feels like a sudden collapse of the future—a descent into fear, uncertainty, and desperate hope.
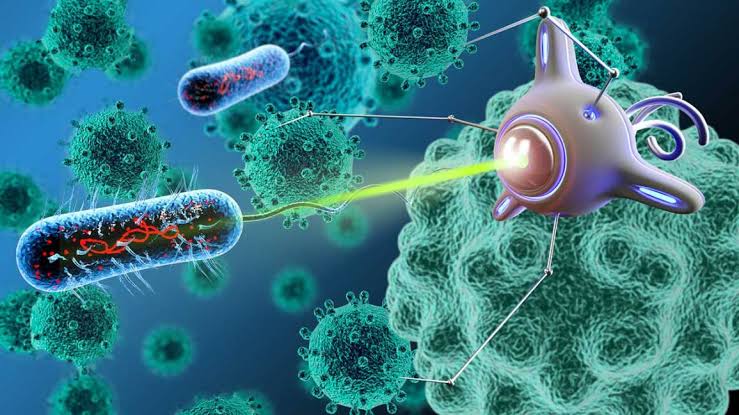
Yet in laboratories around the world, scientists are wielding a revolutionary tool in this battle: nanotechnology. Working at the scale of billionths of a meter, researchers are designing particles smaller than a human cell, capable of navigating the bloodstream, homing in on tumors, and delivering targeted strikes against cancer cells. This is medicine rewritten—not with scalpels and radiation, but with precision machines so small they can slip through the tiniest biological defenses.
Nanotechnology in cancer treatment represents not just incremental progress but a profound transformation of how we understand and fight disease. To grasp its potential, we must first understand the challenges of traditional cancer therapy and how the nanoscale world offers a new frontier of hope.
The Limitations of Traditional Cancer Treatments
Conventional cancer treatments—surgery, chemotherapy, and radiation—have saved countless lives, but they carry harsh limitations. Chemotherapy floods the body with powerful drugs that kill rapidly dividing cells. While effective against cancer, it also harms healthy tissues like hair follicles, bone marrow, and the gastrointestinal tract. This indiscriminate toxicity causes debilitating side effects, from nausea and fatigue to hair loss and weakened immunity.
Radiation therapy, though more localized, can still damage surrounding healthy tissues. Surgery requires invasive procedures and may not reach every malignant cell, particularly in cancers that have spread. Even when these treatments work, recurrence is common because microscopic cancer cells often evade detection.
This is where nanotechnology promises a revolution. Instead of carpet-bombing the body with chemicals, nanoscale medicine can deliver treatments like guided missiles—precise, controlled, and lethal only to cancer cells.
What Is Nanotechnology in Medicine?
Nanotechnology involves manipulating matter at the scale of nanometers, where unique physical and chemical properties emerge. A nanometer is one-billionth of a meter—about 100,000 times smaller than the width of a human hair. At this scale, materials can behave differently: gold nanoparticles can appear red or purple, and carbon can form structures stronger than steel but lighter than plastic.
In medicine, nanotechnology enables the creation of nanoparticles, nanocarriers, and nanodevices capable of interacting with biological molecules in unprecedented ways. Because many biological processes—DNA replication, protein folding, cellular signaling—occur at the nanoscale, nanotechnology can seamlessly integrate with life’s machinery.
For cancer treatment, this means designing particles that can circulate through the bloodstream, bypass immune defenses, recognize cancer cells, and release therapy only where needed. It also enables better imaging and early detection, giving doctors powerful tools to intervene before cancer spreads.
How Nanoparticles Target Cancer Cells
The genius of nanotechnology in oncology lies in its precision. Tumors often have leaky blood vessels with gaps between cells, a phenomenon known as the enhanced permeability and retention (EPR) effect. Nanoparticles can exploit these gaps to slip into tumor tissue more easily than they can enter healthy tissues.
Once inside, nanoparticles can be engineered to recognize molecular markers unique to cancer cells. These markers—proteins or receptors overexpressed on tumor surfaces—act like beacons. Nanoparticles can be coated with ligands, antibodies, or peptides that bind specifically to these markers, ensuring they attach to cancer cells while leaving healthy cells untouched.
This selective targeting dramatically improves drug delivery. Instead of flooding the entire body with chemotherapy, a nanocarrier can deliver a concentrated payload directly to a tumor, reducing systemic toxicity and maximizing therapeutic impact.
Types of Nanoparticles Used in Cancer Therapy
Nanotechnology has birthed a variety of particles and platforms designed to combat cancer. Liposomes, for example, are tiny spherical vesicles made of lipid bilayers that can encapsulate drugs. They are biocompatible and have already reached clinical use, as seen in liposomal doxorubicin formulations that reduce heart toxicity compared to standard chemotherapy.
Polymeric nanoparticles are another versatile platform, made from biodegradable polymers that slowly release drugs over time. Gold nanoparticles can be engineered to absorb specific wavelengths of light, allowing them to heat up and destroy cancer cells through a technique called photothermal therapy. Quantum dots—semiconducting nanocrystals—can help image tumors with exceptional clarity, guiding surgeons and oncologists in real time.
Carbon-based nanomaterials like nanotubes and graphene offer unique mechanical and electrical properties, enabling innovative drug delivery and diagnostic systems. Magnetic nanoparticles, made of iron oxide, can be guided to tumor sites using external magnets and later activated by alternating magnetic fields to generate heat that kills cancer cells—a method called magnetic hyperthermia.
Each of these nanoparticle types can be further functionalized with targeting molecules, stealth coatings to evade immune detection, and responsive triggers that release therapy only under certain conditions (such as acidic pH found in tumors). This multifunctionality makes nanotechnology a powerful, adaptable weapon against cancer.
Nanotechnology in Imaging and Early Detection
Effective cancer treatment depends on early detection. The sooner a tumor is discovered, the better the chances of curing it before it spreads. Nanotechnology enhances this critical stage of oncology by enabling imaging with unprecedented sensitivity.
Nanoparticles can be designed to bind to cancer-specific biomarkers and emit signals detectable by imaging systems like MRI, PET scans, or fluorescence microscopy. For instance, superparamagnetic iron oxide nanoparticles enhance MRI contrast, revealing tumors invisible to conventional scans. Quantum dots can fluoresce brightly under certain lights, helping pathologists identify cancerous cells at the microscopic level.
These innovations move medicine toward a future where cancer can be diagnosed at its earliest, most treatable stages—sometimes even before symptoms arise. Such proactive detection could transform survival rates across many cancer types.
Smart Drug Delivery: Nanocarriers as Guided Therapies
One of the most promising aspects of nanotechnology in cancer treatment is smart drug delivery. Imagine a cancer drug that travels silently through the bloodstream, searching for its target. It remains harmless until it recognizes a tumor cell, then releases its therapeutic cargo precisely where needed.
This is not science fiction but a rapidly advancing field. Nanocarriers can be engineered with multiple layers: an outer coating that disguises them from the immune system, a targeting ligand that recognizes cancer cells, and a core that holds the drug.
Some nanocarriers are even stimuli-responsive. They release their payload only when exposed to certain conditions—such as the acidic environment of tumors, specific enzymes produced by cancer cells, or external triggers like light or heat. This level of control dramatically reduces side effects and allows for higher doses of potent drugs that would otherwise be too toxic.
Examples already in use include Abraxane, a nanoparticle formulation of the chemotherapy drug paclitaxel bound to albumin. It improves drug solubility and delivery while minimizing adverse effects. Research continues into nanoparticles that can carry combinations of drugs, or pair chemotherapy with genetic therapies like siRNA, delivering multi-pronged attacks within a single nanoscale package.
Nanotechnology and Immunotherapy
The immune system is our natural defense against disease, yet cancer cells evolve cunning strategies to evade detection. Immunotherapy seeks to reawaken the body’s immune response to fight cancer, and nanotechnology is proving to be a crucial ally.
Nanoparticles can deliver immune-activating agents directly to lymph nodes or tumor sites, training immune cells to recognize and attack cancer. They can also transport checkpoint inhibitors—drugs that block proteins used by cancer cells to suppress immunity—more efficiently, reducing systemic side effects.
Researchers are exploring nanovaccines, tiny particles carrying tumor antigens that stimulate a targeted immune response. These personalized nanovaccines could one day be tailored to each patient’s unique cancer profile, mobilizing their immune system with unprecedented precision.
Overcoming Drug Resistance with Nanotechnology
One of the deadliest traits of cancer is its ability to adapt and resist treatment. Tumors can develop mechanisms that pump drugs out of cells, alter drug targets, or repair DNA damage caused by therapies.
Nanotechnology offers ways to bypass these defenses. By packaging drugs in nanoparticles, scientists can sneak past resistance mechanisms, ensuring therapeutic molecules reach their intended targets. Nanocarriers can also co-deliver drugs that work synergistically, preventing cancer cells from adapting.
In some designs, nanoparticles physically disrupt cell membranes or release agents that disable drug-resistance proteins. These strategies re-sensitize tumors to treatment, reviving drugs that had become ineffective.
Photothermal and Photodynamic Nanotherapies
Beyond delivering drugs, nanoparticles can destroy cancer cells through novel physical mechanisms. Photothermal therapy uses nanoparticles that absorb near-infrared light and convert it into heat. When these particles accumulate in tumors and are activated by an external laser, they heat up and selectively kill cancer cells without harming surrounding tissue.
Photodynamic therapy takes a different approach. Nanoparticles carry light-sensitive compounds that, when illuminated, produce reactive oxygen species toxic to cancer cells. Combining nanocarriers with these therapies improves their delivery and effectiveness, opening new paths for non-invasive cancer treatments.
Real-World Impact and Clinical Progress
Nanotechnology is not just a futuristic vision—it is already making a difference. Several nanoparticle-based cancer drugs have received FDA approval, improving outcomes for patients with breast cancer, ovarian cancer, and other malignancies. Clinical trials are underway for many more, exploring nanoparticles for imaging, targeted drug delivery, and combination therapies.
In real-world cases, patients treated with nanomedicine formulations often experience fewer side effects and improved quality of life compared to traditional chemotherapy. Nanotechnology has also enabled breakthroughs in treating cancers once considered intractable, offering new hope to patients who had exhausted other options.
Challenges and Ethical Considerations
Despite its promise, nanotechnology faces hurdles. Manufacturing nanoparticles consistently and safely at scale is complex. Understanding long-term effects, including how nanoparticles are metabolized or cleared from the body, requires ongoing research. There are concerns about potential toxicity or unintended interactions with healthy tissues.
Ethical questions also arise: Who will have access to these advanced treatments? Will they be affordable or deepen global health inequities? As with any powerful technology, ensuring responsible development and equitable distribution is crucial.
The Future: Toward a Nanocure for Cancer
The future of nanotechnology in oncology is breathtaking. Scientists envision nanoparticles that patrol the body continuously, detecting cancer cells at their inception and eradicating them before a tumor forms. Artificial intelligence could design bespoke nanocarriers tailored to each patient’s genetics and cancer profile.
Hybrid nanoparticles may combine multiple functions: detecting tumors, delivering therapy, monitoring response, and even self-destructing after their mission is complete. Gene-editing tools like CRISPR could be delivered via nanoparticles to directly repair mutations driving cancer.
Ultimately, nanotechnology may transform cancer from a deadly disease into a manageable or even preventable condition. While a universal cure remains elusive, every advancement brings us closer to a world where a cancer diagnosis no longer strikes fear but signals a treatable challenge.
A Hope Measured in Nanometers
In the battle against cancer, hope has often come in large, dramatic interventions—major surgeries, powerful drugs, aggressive radiation. Nanotechnology shifts this paradigm. It offers a vision of healing not through overwhelming force, but through elegance, precision, and a deep understanding of life at its smallest scales.
For patients and families, this means a future where treatments are kinder, outcomes brighter, and survival more certain. The nanoscale revolution is not just about science—it is about restoring time, health, and dignity to millions of lives touched by cancer.
As researchers continue to unlock the secrets of the nanoworld, we move closer to rewriting the story of cancer. What was once an unstoppable foe may one day be subdued by machines too small to see, yet powerful enough to save a life. This is the promise of nanotechnology: hope measured in nanometers, changing medicine forever.