For centuries, the ritual of diagnosis began the same way. A patient walks into a clinic, sits across from a doctor, and tells their story. The doctor listens, observes, touches, and interprets. Stethoscope to chest, hand to forehead, eyes narrowed in contemplation—it’s an art as much as a science. For much of human history, diagnosis has been an act of personal intimacy, shaped by training, experience, and human intuition.
But something is changing.
Today, in exam rooms and hospitals across the world, a new kind of intelligence is joining the conversation. It doesn’t wear a white coat. It doesn’t sleep. It processes in seconds what would take a lifetime for any human brain. This new partner is artificial intelligence—AI—and it’s reshaping the way doctors diagnose disease.
Not with cold detachment, as some might fear, but with the power to see patterns invisible to the human eye, to catch whispers of illness in oceans of data, and to offer doctors not replacements—but extensions of their minds. This is not the future. This is now.
The Pulse Beneath the Algorithm
To understand how AI is revolutionizing diagnosis, we must first grasp what diagnosis actually is. It’s not just naming a disease—it’s solving a mystery. A good diagnosis is a detective story, and the body is both crime scene and witness. The clues are varied: a high fever, a shadow on a scan, a mutation in a gene, a strange rash, a faint murmur in the heart. The doctor’s role is to gather these signals and interpret them correctly.
But here’s the challenge: modern medicine has become unimaginably complex. Thousands of diseases, millions of data points, rapidly evolving knowledge, and limited time per patient make it nearly impossible for even the best-trained minds to keep up.
AI thrives in this chaos.
Unlike a human, AI doesn’t tire, doesn’t forget, and doesn’t have bias—at least not unless it’s trained with one. A well-designed AI system can sift through terabytes of patient data, cross-reference it with the latest medical literature, and return a ranked list of likely diagnoses in seconds.
In other words, AI listens faster, learns wider, and remembers more. When used ethically and responsibly, it doesn’t undermine the doctor’s art—it strengthens it.
Radiology: Seeing Beyond the Visible
One of the earliest and most impactful uses of AI in diagnosis has been in radiology. Radiologists examine X-rays, CT scans, MRIs, and other images to detect abnormalities—tumors, fractures, blood clots, signs of infection. But reading these images is a skill honed over years of training, and even the best radiologists can occasionally miss subtle signs.
Enter the algorithm.
AI systems like Google Health’s DeepMind or Zebra Medical Vision have shown remarkable ability to identify diseases in medical images—sometimes with greater accuracy than human experts. These systems are trained on millions of anonymized images, learning to detect minute patterns that might escape the human eye.
For instance, an AI can analyze a mammogram and detect early signs of breast cancer that might be missed by radiologists, especially in dense breast tissue. In diabetic retinopathy, AI has achieved near-perfect accuracy in spotting early changes in the retina that can lead to blindness if untreated.
But the goal isn’t to replace radiologists. Instead, AI acts like a digital co-pilot—flagging potential issues, suggesting areas of concern, and helping doctors focus their expertise where it’s needed most.
Voice of the Machine in the Clinic
Even outside of imaging, AI is changing how diseases are diagnosed during routine doctor visits. Natural language processing (NLP)—a field of AI that allows computers to understand and interpret human language—is being used to analyze patient speech, doctor notes, and even conversations during exams.
Imagine a patient describing symptoms to a voice-enabled system. As they speak, the AI listens—not just to the words, but to the tone, cadence, pauses, and emotional cues. It compares this information with thousands of similar cases, helping to highlight possible diagnoses. It also automatically transcribes notes for the physician, freeing up valuable time and reducing errors in documentation.
Companies like Nuance (now part of Microsoft) and startups like Abridge are already deploying such technology in hospitals. They aim to lift the burden of data entry and empower physicians to do what they do best—connect with the patient.
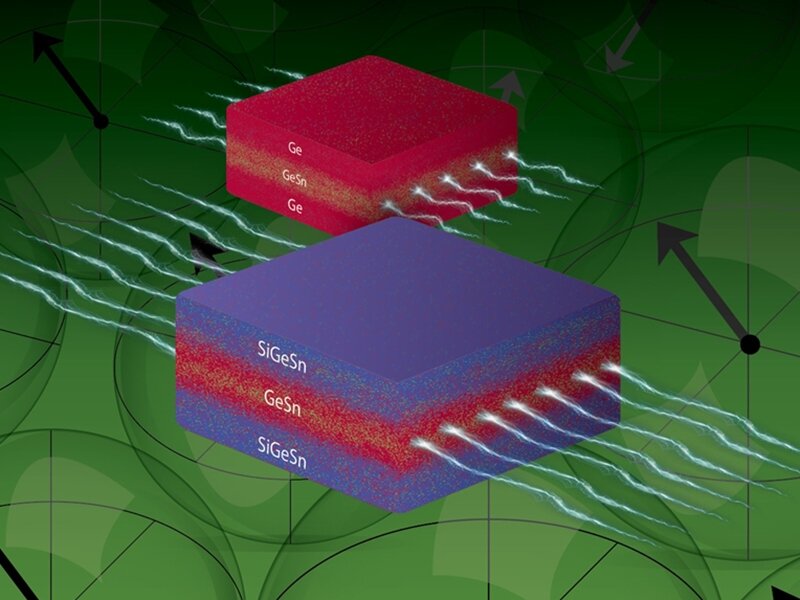
The Genetics Revolution
One of the most powerful areas where AI is reshaping diagnosis lies deep within us: our DNA. Genomic medicine—decoding the information in our genes—has exploded in recent years. Sequencing an entire human genome now costs less than a high-end smartphone. But interpreting that genome? That’s where the real challenge lies.
A single genome contains over three billion base pairs. Finding which of those might be linked to a rare disease is like finding a typo in a library of a million books.
AI is a perfect partner here.
Tools like DeepVariant (developed by Google) can accurately detect genetic variants from sequencing data. AI can spot mutations, predict their effects, and even suggest potential treatments based on other similar cases worldwide. For children born with undiagnosed disorders, AI-driven genomic analysis can often mean the difference between years of uncertainty and a clear diagnosis.
More astonishingly, AI is starting to interpret the “junk” DNA—the vast stretches once thought useless but now known to regulate important biological functions. As AI dives deeper into these genomic mysteries, new causes of disease are emerging—sometimes in places no human ever thought to look.
Infectious Disease and Outbreak Prediction
When COVID-19 swept across the globe in 2020, it exposed many cracks in our healthcare systems. But it also showcased how AI could be mobilized to track, predict, and even help diagnose viral infections.
Early in the pandemic, AI tools were used to analyze lung scans to detect COVID-19-related pneumonia. Chatbots screened millions of people for symptoms, triaged them, and directed them to care. In some hospitals, AI helped monitor patients’ oxygen levels, flagging deteriorations before nurses could intervene.
AI also played a vital role in understanding the virus’s spread. Machine learning models analyzed flight data, cellphone movements, and social media trends to predict hotspots. Companies like BlueDot even used AI to issue early warnings about the outbreak—days before traditional global health organizations.
In a world where new diseases can emerge overnight, AI offers a way to diagnose and contain threats at lightning speed.
Psychiatry and the Invisible Wounds
Diagnosing mental health disorders has always been challenging. Unlike infections or tumors, depression doesn’t show up on a scan. Anxiety doesn’t cause a fever. Bipolar disorder doesn’t leave a biochemical fingerprint—at least not one we can easily detect.
Here too, AI is making inroads. By analyzing speech patterns, facial expressions, typing behavior, and even smartphone usage, AI can detect subtle signs of depression, cognitive decline, or manic episodes. For example, decreased vocabulary, longer pauses, and flat vocal tone may indicate early stages of Alzheimer’s or major depression.
These tools are still in development, and ethical concerns abound. But they offer the hope of earlier detection, personalized monitoring, and timely intervention—especially in communities where psychiatrists are scarce.
Personalized Diagnosis in a Crowded World
Every patient is different. Two people with the same disease may present with different symptoms, respond to different treatments, and recover at different speeds. Traditional medicine, based on population averages, struggles with this variability.
AI thrives on individualization.
By integrating data from wearables, medical records, genetic tests, lifestyle, environment, and even social determinants of health, AI can create a “digital twin” of a patient—a virtual model that simulates their biology. Doctors can then test treatments in this twin before trying them on the real patient. It’s a radical leap toward truly personalized medicine.
For chronic diseases like diabetes, heart failure, or asthma, AI-powered apps now predict flare-ups before they occur, nudging patients to take action early. These systems don’t just diagnose—they anticipate.
The Ethics of Machines in Medicine
As with all revolutions, the rise of AI in diagnosis brings risks. Algorithms are only as good as the data they’re trained on. If that data reflects racial, gender, or socioeconomic biases—as much of healthcare data historically has—the AI can perpetuate and amplify those biases.
There are stories where AI systems misdiagnosed Black patients at higher rates or failed to recognize rare diseases in women because the training datasets were predominantly male or white. Transparency, diversity in datasets, and strict ethical oversight are not optional—they’re essential.
And what about trust? Patients trust doctors because they’re human, because they care, because they can explain their thinking. When an AI recommends a diagnosis, can we explain how it reached that conclusion? This issue—AI interpretability—is one of the biggest challenges in the field.
Still, the consensus is growing: AI should not replace doctors. It should enhance them. A powerful tool in the hands of a compassionate, trained human becomes more than a machine. It becomes a force for healing.
Doctors, Not Robots
Despite headlines, the heart of diagnosis will always belong to humans. AI doesn’t sit with a patient and feel their fear. It doesn’t notice the nervous tapping of a foot, the fleeting glance of worry, or the subtle silence that follows bad news. It doesn’t cradle a hand or say, “I understand.”
But paired with a doctor, AI becomes something powerful. The machine brings memory, precision, and speed. The doctor brings empathy, wisdom, and ethical judgment. Together, they are more than either could be alone.
We’re not replacing the healer. We’re giving them superpowers.
A Future Whispering Through Wires
As we move deeper into the 21st century, diagnosis is transforming from an art built on intuition to a science powered by code. Hospitals will be filled with sensors. Our smartphones will become early warning systems. Diseases may be caught not when we feel sick—but before we feel anything at all.
This new world is not without risks. But it is full of promise.
Imagine a mother in a rural village whose child develops a strange rash. With a single photo, AI guides her to the right diagnosis and treatment—saving the child’s life. Imagine an elderly man whose cough is dismissed as age—but AI detects early lung cancer. He lives because the machine saw what the human eye missed.
Imagine your own story—your future health, your family’s well-being—touched by a partnership between mind and machine.
The stethoscope may still hang around the neck. But inside the clinic, whispering behind every diagnosis, is something new. An intelligence that doesn’t replace human care—but helps it become more human than ever.