For centuries, women had little control over the timeline of their fertility. Biological clocks ticked silently, sometimes clashing with personal goals, careers, relationships, or health challenges. In recent decades, however, science has opened a new chapter: egg freezing, or oocyte cryopreservation. Once considered experimental, egg freezing has now emerged as a powerful tool that allows women to preserve fertility and expand choices for the future.
But this is not simply a medical procedure—it is an emotional, deeply personal decision that intertwines science, hope, empowerment, and uncertainty. For some, it represents freedom. For others, a backup plan. And for many, it is an anchor of reassurance in an unpredictable world.
This guide explores egg freezing in its full scope: the science behind it, the reasons women choose it, the process itself, the risks, the costs, and the emotional journey that accompanies it. Whether you are considering egg freezing for yourself, supporting a loved one, or simply curious, understanding the complexities of this option can help transform what feels overwhelming into clarity.
What Is Egg Freezing?
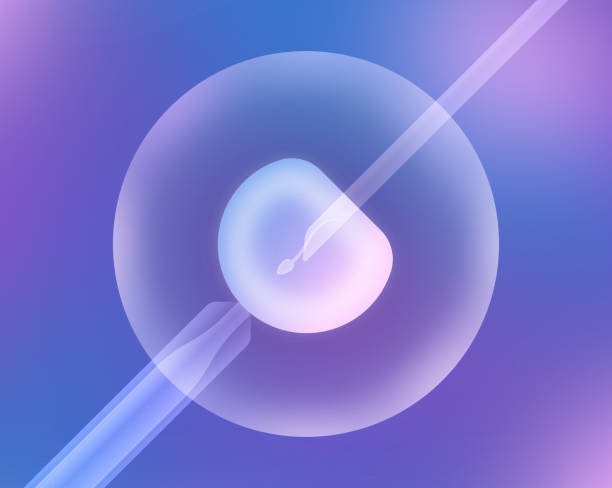
Egg freezing is the process of retrieving a woman’s eggs (oocytes), freezing them at an extremely low temperature, and storing them for future use. When or if the woman is ready to conceive later in life, the eggs can be thawed, fertilized with sperm, and implanted in the uterus through in vitro fertilization (IVF).
The freezing itself is a marvel of modern science. Eggs are delicate and sensitive to ice crystal formation, which can damage them. To solve this, doctors use a method called vitrification—an ultra-rapid freezing process that turns the egg into a glass-like state without forming damaging crystals. This advancement has significantly improved survival rates after thawing, making egg freezing a viable option for fertility preservation.
Why Women Choose to Freeze Their Eggs
The decision to freeze eggs is never made lightly. It often arises from a mixture of personal, professional, and medical considerations.
For many, it is about timing. Women today may pursue advanced education, build careers, travel, or wait to find the right partner before starting a family. Yet, fertility declines with age—particularly after age 35—making the window for natural conception narrower than many realize. Egg freezing offers a way to pause that clock.
For others, it is about medical necessity. Women facing cancer treatments such as chemotherapy or radiation may choose to freeze eggs beforehand, since these therapies can damage ovarian function. Similarly, those with conditions like endometriosis or a family history of early menopause may use egg freezing as a safeguard against future infertility.
And then there are women who simply want reassurance. They may not know if they will ever need to use their frozen eggs, but the option itself provides peace of mind—a way to reduce anxiety about a future filled with uncertainties.
The Role of Age in Egg Freezing
Age is perhaps the single most important factor in the success of egg freezing. A woman is born with all the eggs she will ever have, and both the quantity and quality decline with time. By the late 20s, fertility gradually declines. By the mid-30s, the decline accelerates. By 40, the chances of conceiving naturally are significantly reduced, and the risk of genetic abnormalities increases.
This means that while egg freezing is possible at almost any reproductive age, outcomes are better when it is done earlier. Eggs retrieved at age 28 will generally have higher quality than eggs retrieved at age 38. This does not mean egg freezing is only worthwhile in youth, but it does highlight the importance of timing.
Doctors often advise that the “optimal window” for egg freezing is between ages 28 and 35, though women in their late 30s can still benefit depending on their ovarian reserve and health. Understanding one’s fertility through tests like AMH (anti-Müllerian hormone) levels or antral follicle counts can help guide this decision.
The Egg Freezing Process: Step by Step
The process of egg freezing can feel intimidating at first glance, but understanding each step demystifies it.
Initial Consultation
The journey begins with a fertility specialist. At the consultation, the doctor reviews medical history, performs blood tests, and often conducts an ultrasound to evaluate ovarian reserve. This step helps determine how many eggs might be retrieved and what kind of stimulation protocol will be used.
Ovarian Stimulation
Because a woman naturally releases just one egg per month, fertility specialists use hormonal medications to stimulate the ovaries into producing multiple eggs at once. This stage lasts 10–14 days and involves daily hormone injections. Patients are closely monitored through ultrasounds and blood work to track follicle growth.
During this period, women often experience physical symptoms—bloating, mood changes, or fatigue—as hormone levels rise. Emotionally, it can feel like a rollercoaster, balancing excitement, anxiety, and physical discomfort.
Egg Retrieval
Once the follicles are mature, egg retrieval is scheduled. This is a short outpatient procedure performed under sedation. Using ultrasound guidance, a thin needle is inserted through the vaginal wall to collect the eggs. The procedure usually lasts 20–30 minutes, and recovery is relatively quick.
The number of eggs retrieved varies from person to person, depending on age and ovarian reserve. Some women may retrieve only a handful, while others may retrieve 20 or more.
Freezing and Storage
After retrieval, the eggs are evaluated for maturity. Only mature eggs are frozen through vitrification and stored in specialized tanks filled with liquid nitrogen at –196°C. Here, time effectively stops for the eggs—they can remain frozen for years, even decades, without deteriorating.
Success Rates: What the Numbers Really Mean
A critical question for anyone considering egg freezing is: How likely is it to work? Success rates depend on several factors—especially the woman’s age at the time of freezing and the number of eggs retrieved.
Research shows that younger women typically require fewer eggs to achieve a successful pregnancy later. For example, freezing 15–20 eggs before age 35 may provide a 70–80% chance of at least one live birth. In contrast, women freezing eggs at age 38 or older may need more eggs for a similar chance.
It is important to recognize that egg freezing does not guarantee a baby. It increases the odds but cannot overcome all factors that influence fertility, such as sperm quality, uterine health, or genetic issues.
Emotional Dimensions of Egg Freezing
Beyond science, egg freezing is a deeply emotional experience. Some women describe it as empowering—the ability to take control of their reproductive future. Others find it stressful, confronting the realities of fertility decline or navigating the pressure of making a costly, time-sensitive decision.
There is also an emotional complexity in deciding when to use frozen eggs. For some, frozen eggs remain untouched because they conceive naturally. For others, those eggs become the only pathway to parenthood.
Support systems—friends, family, or therapists—play a vital role during this journey. Fertility specialists often encourage women to approach the process with realistic expectations: to view egg freezing as a backup option, not a promise.
Risks and Side Effects
Like any medical procedure, egg freezing carries risks. Ovarian stimulation can sometimes lead to ovarian hyperstimulation syndrome (OHSS), a condition where the ovaries swell and leak fluid. Though rare with modern protocols, it can cause discomfort or, in severe cases, hospitalization.
The egg retrieval procedure itself carries minimal risks, such as bleeding or infection, but these are uncommon. Long-term studies show no significant increase in cancer or other major health risks associated with egg freezing.
Emotionally, the risks include disappointment or regret—if not enough eggs are retrieved, if thawing does not succeed, or if pregnancy is not achieved later. This underscores the importance of informed decision-making and managing expectations.
Costs and Accessibility
One of the most significant barriers to egg freezing is cost. In many countries, a single cycle can range from $6,000 to $15,000 or more, not including medications, which may add several thousand dollars. Storage fees, usually charged annually, add further costs.
Because success often requires multiple cycles to collect enough eggs, total expenses can climb quickly. Insurance coverage is limited in many places, though some employers now offer fertility benefits. Accessibility varies widely by geography, with egg freezing available in major urban centers but less so in rural or underserved areas.
For many women, the financial burden can be as challenging as the physical or emotional aspects of the journey.
When and How Frozen Eggs Are Used
When a woman is ready to use her frozen eggs, they are thawed in the laboratory. Not all eggs survive the thawing process, but with modern vitrification techniques, survival rates are high.
Next, the eggs are fertilized with sperm, often through intracytoplasmic sperm injection (ICSI), where a single sperm is injected into the egg. The resulting embryos are monitored for growth, and the healthiest are selected for transfer to the uterus.
Pregnancy rates depend not only on the quality of the eggs but also on the woman’s uterine health, overall health, and partner or donor sperm quality.
Ethical and Social Considerations
Egg freezing is not just a medical option; it also carries ethical and societal implications. Some critics worry that egg freezing may give women false reassurance, delaying parenthood in ways that could reduce overall fertility outcomes. Others argue that it empowers women by aligning reproductive choices with modern lifestyles.
There are also questions about who should have access. Should egg freezing be offered only for medical reasons, like cancer patients, or also for “social reasons,” like career planning? Should storage have time limits? And what happens to unused eggs?
These debates reflect the complexity of combining science with deeply personal life choices.
The Future of Egg Freezing
Egg freezing is still evolving. Scientists are exploring ways to improve ovarian stimulation, refine freezing techniques, and even develop artificial ovaries. Advances in reproductive genetics may one day allow eggs to be tested for health before freezing, further improving success rates.
As societal acceptance grows, egg freezing may become as common as other reproductive choices like IVF. Already, some companies offer it as part of employee benefits, framing it as an investment in women’s futures.
The future may bring not only improved outcomes but also greater accessibility, helping ensure that egg freezing is not a privilege for the few but an option for many.
The Personal Journey
Ultimately, egg freezing is about more than science or statistics—it is about individual lives, dreams, and uncertainties. For some women, it is a life-changing decision that brings relief and possibility. For others, it may remain a path never taken.
Each story is unique. A woman in her early 30s, balancing career and relationships, may see egg freezing as empowerment. A young cancer patient may see it as hope. A woman who froze eggs at 35 and later used them at 42 may see it as her bridge to motherhood.
The unifying thread is choice. Egg freezing does not dictate the future, but it widens the horizon of possibilities.
Conclusion: A Science of Hope
Egg freezing is one of the most profound intersections of science and human desire. It is the science of preserving potential, the hope of future family, the freedom to align parenthood with life’s unpredictable paths.
It is not without challenges—financial, physical, emotional—but for many, it is worth the effort. Egg freezing cannot promise a child, but it can offer time, reassurance, and possibility.
In the end, egg freezing is not about stopping time but about reclaiming it. It allows women to carry forward a piece of their present into the future, a reminder that while biology sets limits, science can expand choices. And in those choices lies a new kind of freedom—the freedom to decide when, why, and how to embrace the journey of parenthood.