There are moments in life when time is not just precious—it’s everything. In the realm of cancer, early detection can make the difference between life and death, between a curable disease and an unstoppable one. Yet for many, the idea of cancer screening still feels distant, confusing, or even frightening. The machines, the tests, the waiting, the unknown—it can all feel like too much. But knowledge can be more powerful than fear. And understanding cancer screening is a first step toward saving lives—not just others’, but possibly your own.
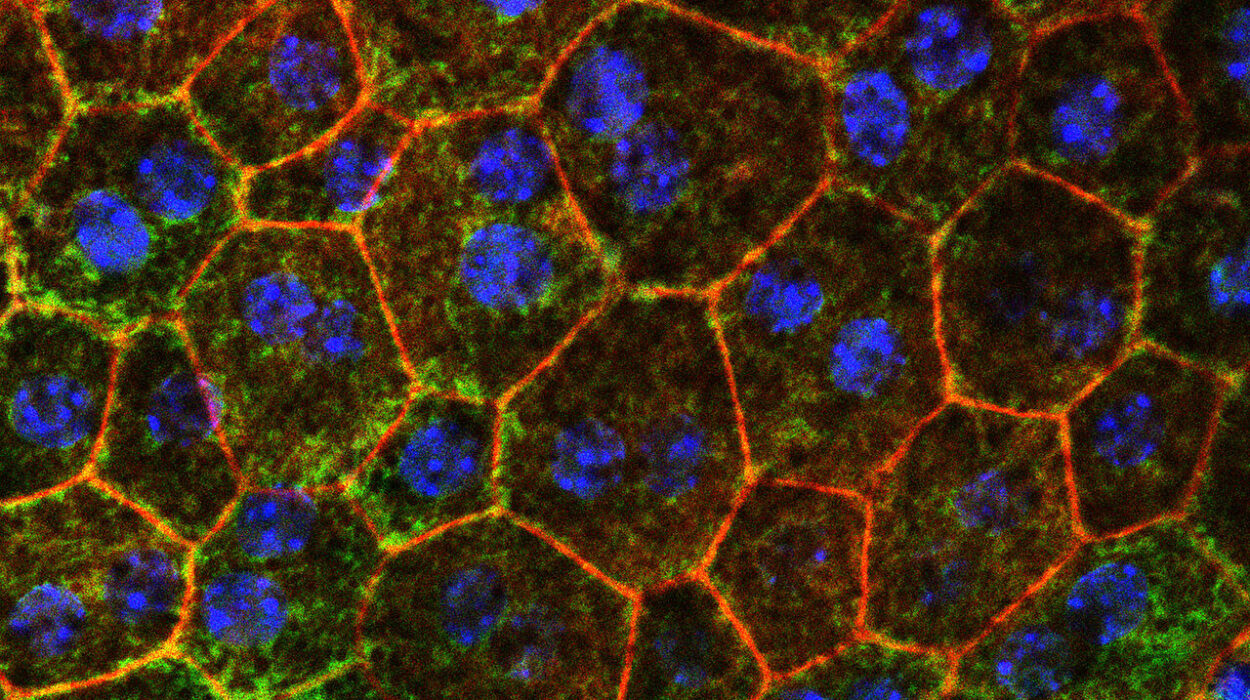
Cancer does not begin with pain. It begins silently. A single cell mutates and begins to divide without control, slipping past the body’s defenses. It may take years for symptoms to appear. By the time we feel something is wrong, cancer may already be spreading its roots deep within. This is where screening becomes a quiet hero—catching what we cannot yet feel, offering hope long before symptoms ever begin.
What Screening Actually Means
Cancer screening is not about diagnosing a disease that is already showing itself. It is about searching for signs of cancer before any symptoms arise. Screening looks for early changes—abnormal cells, small growths, subtle blood changes—that could suggest a problem is beginning. The goal is not just to find cancer, but to find it early enough to treat it effectively.
It’s not guesswork. Screening is based on decades of research and statistical understanding. It is targeted to specific cancers, designed for certain age groups, and recommended for people with specific risk profiles. Not everyone needs every test. But for the right person, at the right time, a screening can be a gift of years.
There’s also a difference between screening and diagnostic testing. Screening is proactive and often done in healthy people. Diagnostic tests are reactive, used when there’s already a reason to suspect cancer—like a lump, blood in the stool, or abnormal bleeding. Both are vital. Both can save lives.
The Fear Factor
So why do people avoid screening? The reasons are as complex as human psychology. Some are afraid of the results. Others feel they are too busy. Some don’t know which tests they need or how to ask. Misinformation, stigma, cost, and even cultural silence around cancer all play a role. Many people still think cancer is a death sentence—so they avoid knowing if it’s there.
But fear doesn’t stop cancer. Silence doesn’t keep us safe. The truth is, many cancers are highly treatable when caught early. In fact, some can even be prevented entirely by removing pre-cancerous tissue. The earlier we look, the better the odds.
Breast Cancer: A Matter of Awareness
Breast cancer is one of the most well-known, and yet still misunderstood, cancers. It’s the most common cancer in women worldwide. But thanks to awareness campaigns and improved technology, survival rates are climbing—especially for women who undergo regular screening.
The most common screening test is the mammogram—an X-ray of the breast that can detect tumors too small to be felt. It’s not always comfortable, and sometimes the results can be unclear. But when used routinely, mammograms have been proven to reduce breast cancer deaths significantly.
Newer technologies like 3D mammography (digital breast tomosynthesis) offer clearer images and reduce false positives. Ultrasound and MRI can help when mammograms aren’t enough, particularly in women with dense breast tissue or high genetic risk.
And risk matters. Women with a family history of breast or ovarian cancer, or known BRCA1/BRCA2 gene mutations, may need earlier and more frequent screenings. Understanding your personal risk profile is as important as the tests themselves.
Cervical Cancer: A Story of Prevention
Cervical cancer used to be a leading cause of death for women. Today, it is one of the most preventable forms of cancer—thanks to screening and vaccination.
The Pap test (or Pap smear) looks for precancerous changes in the cells of the cervix. It is simple, quick, and often life-saving. Alongside the Pap, the HPV test checks for high-risk strains of the human papillomavirus—especially types 16 and 18, which cause most cervical cancers.
HPV is so common that nearly all sexually active people are exposed at some point. For most, the virus clears naturally. But in some, it lingers—and that’s when risk begins.
The beauty of cervical cancer screening is that it doesn’t just catch cancer early—it often catches the stage before cancer, when treatment is as simple as removing a patch of abnormal cells. This is prevention in its purest form.
The HPV vaccine, recommended for preteens and young adults, adds another powerful layer of protection. The combination of vaccine and screening has the potential to eliminate cervical cancer as a public health threat. But only if people keep showing up for the tests.
Colon Cancer: The Silent Invader
Colon cancer doesn’t announce its arrival with pain or visible signs. It grows quietly, often from small polyps—benign growths that can become cancerous over time. Screening for colon cancer is not just detection—it is interception.
Colonoscopy remains the gold standard. During this test, a flexible camera is guided through the colon, and any polyps found can be removed on the spot. It’s a powerful act of prevention and diagnosis in one.
Other tests exist: the fecal immunochemical test (FIT), guaiac-based fecal occult blood test (gFOBT), and stool DNA tests like Cologuard. These check for hidden blood or abnormal DNA in stool. While less invasive than colonoscopy, they are also less precise and need to be done more often.
The risk of colon cancer rises with age. That’s why guidelines typically recommend starting screening at 45 for average-risk adults. For those with a family history, inflammatory bowel disease, or certain genetic syndromes, earlier and more frequent testing may be needed.
When caught early, colon cancer is highly curable. When caught late, it can be deadly. The difference is often a single test, done on time.
Lung Cancer: Catching It Before It Kills
For decades, lung cancer was a silent killer. By the time symptoms like coughing or weight loss appeared, the disease was often advanced. But now, for people at high risk, there is hope in early detection.
Low-dose computed tomography (LDCT) is a special type of CT scan that can detect lung cancer at earlier, more treatable stages. It’s recommended for adults aged 50 to 80 who have a significant smoking history—typically 20 pack-years or more—and who currently smoke or quit within the last 15 years.
Unlike traditional chest X-rays, which miss many early tumors, LDCT has been shown to reduce lung cancer deaths by catching the disease before it spreads. It’s not for everyone—just for those with elevated risk. But for that group, it’s a game changer.
Lung cancer screening is still underused, partly due to stigma. Smokers often feel shame or guilt and may avoid testing. But cancer is not a moral failure. It is a disease, and it deserves early attention like any other.
Prostate Cancer: Between Vigilance and Caution
Prostate cancer is one of the most common cancers in men, particularly over the age of 50. But it’s also one of the most controversial when it comes to screening. The balance between benefit and harm is delicate.
The main screening tool is the prostate-specific antigen (PSA) blood test. Elevated PSA levels can indicate cancer, but also benign conditions like prostatitis or an enlarged prostate. False positives can lead to unnecessary biopsies and anxiety.
That’s why screening decisions are now personalized. Men are encouraged to discuss the pros and cons of PSA testing with their healthcare providers, especially if they’re between 50 and 69. African American men and those with a family history of prostate cancer may need earlier screening.
Recent advancements include more precise PSA derivative tests, MRI before biopsy, and genomic profiling of prostate tissue. These tools help distinguish slow-growing cancers that may be monitored from aggressive ones that require treatment.
Prostate cancer is often slow, but not always. When aggressive, it can metastasize quickly. The key is informed, individualized screening—not a one-size-fits-all approach.
Skin Cancer: The Most Visible, and Still Overlooked
Of all cancers, skin cancer is the most visible and the most common. Yet people still ignore suspicious moles, dismiss new lesions, or put off dermatology visits. Part of the problem is that skin cancer often doesn’t feel dangerous—until it is.
There are three major types: basal cell carcinoma, squamous cell carcinoma, and melanoma. The first two are usually treatable with early detection. Melanoma, though rarer, is far more aggressive and deadly if caught late.
Screening for skin cancer involves full-body visual exams, either self-conducted or done by a dermatologist. People at high risk—those with fair skin, many moles, family history, or extensive sun exposure—should be especially vigilant.
The ABCDEs of melanoma (Asymmetry, Border, Color, Diameter, Evolution) are easy to remember and can save lives. But even better is seeing a professional for regular skin checks. One look from a trained eye can catch what we overlook.
Blood, Bones, and Beyond
Some cancers don’t have standardized screening tools—yet. Blood cancers like leukemia and lymphoma are typically diagnosed after symptoms arise. But routine blood counts and awareness of fatigue, infections, or unusual bruising can help.
Pancreatic cancer, one of the most lethal, is often detected too late. Researchers are racing to find early biomarkers, with promising leads in blood-based genetic and protein tests. Ovarian cancer, too, lacks a reliable screening method, though pelvic exams, transvaginal ultrasounds, and CA-125 blood tests are sometimes used in high-risk women.
Emerging technologies like liquid biopsies—blood tests that detect cancer DNA—are on the horizon. These could eventually allow for multi-cancer early detection from a single vial of blood. But for now, most are still under investigation or used in specific clinical scenarios.
Bone scans, PET scans, and advanced imaging are valuable in diagnosing and staging known cancers, especially when doctors suspect metastasis. These are not screening tools, but they are vital in determining how far cancer has spread and how best to treat it.
The Emotional Terrain
Screening is not just a medical procedure. It is an emotional experience. The moment you lie down for a scan or wait for a call from your doctor, the world can feel suspended. Time stretches, imagination runs wild, and anxiety blooms in the silence.
This emotional toll is real and valid. So is the courage it takes to walk into a clinic knowing what might be found. But the alternative—remaining unaware—is more dangerous.
It’s also important to remember that most screenings do not lead to a cancer diagnosis. Many come back normal. Others catch problems early. And even when cancer is found, early detection can turn panic into a plan.
Doctors, nurses, and techs understand this landscape. Many are trained not just in the science, but in the human element—reassuring words, gentle hands, clear explanations. Don’t hesitate to ask questions or express your fears. You are not alone in this.
Taking Charge of Your Own Timeline
One of the most powerful things you can do for your future self is to get screened. It’s a vote for life—a decision that ripples across years. When you schedule a mammogram, a colonoscopy, or an HPV test, you’re not just reacting to fear. You’re taking control. You’re declaring that your life matters enough to check.
Talk to your doctor. Ask what screenings are right for your age, gender, family history, and lifestyle. Keep a calendar. Encourage your loved ones to do the same. Make it normal to talk about these things—at dinner, on the phone, at school or work. Cancer is not shameful. Screening should not be rare.
Science, Progress, and the Path Ahead
We live in an era of breathtaking progress. Genetic testing can identify inherited cancer risks before disease starts. Artificial intelligence is improving imaging accuracy. Researchers are developing wearable devices that monitor for tumor markers. The future of cancer screening is not static—it is evolving rapidly, and with great promise.
But the most effective test is still the one you actually take. The best prevention is the one you act on. Science provides the tools. It’s up to us to use them.
In the end, cancer screening is not about statistics. It is about people—mothers, fathers, siblings, friends—getting more time, more birthdays, more memories. It is about a future that doesn’t vanish in silence but is spoken for, tested for, fought for.
And maybe, one day, it’s about hearing a doctor say: “We caught it early. You’re going to be okay.”