Parkinson’s disease is more than a medical term—it is a human story. It is the story of a progressive neurological condition that touches not only the lives of those who carry it but also the families, friends, and caregivers who walk alongside them. Named after Dr. James Parkinson, who first described it in 1817 as the “shaking palsy,” Parkinson’s disease remains both a scientific mystery and a deeply human challenge.
This condition affects movement, but it also influences emotions, cognition, and daily life in ways that extend far beyond physical symptoms. To understand Parkinson’s disease is to look at it through multiple lenses: the biological changes unfolding inside the brain, the lived experiences of individuals, the progress of science toward treatments, and the ongoing hope for a cure.
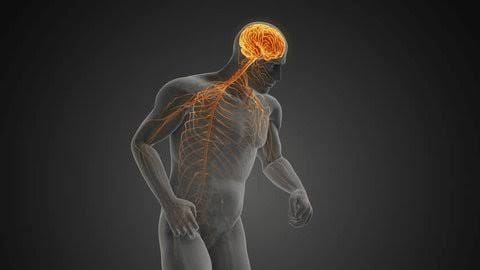
The Brain at the Center of It All
At the heart of Parkinson’s disease lies the brain, specifically an area known as the substantia nigra, which plays a critical role in controlling movement. In healthy brains, specialized neurons in this region produce dopamine, a chemical messenger that transmits signals between nerve cells to coordinate smooth, purposeful motion.
In Parkinson’s disease, these dopamine-producing neurons gradually die off. As dopamine levels drop, communication between different regions of the brain begins to falter. Movements that were once automatic—walking, writing, speaking—become slower, stiffer, and more difficult. Over time, the shortage of dopamine disrupts not only movement but also mood, motivation, and even memory.
The loss of these neurons is progressive, meaning it worsens over time, and currently, science does not fully understand why. This slow and relentless degeneration is what makes Parkinson’s disease both uniquely challenging and deeply impactful.
Causes of Parkinson’s Disease: What We Know and What We Don’t
One of the most difficult truths about Parkinson’s disease is that its exact cause remains elusive. Scientists know that it results from the loss of dopamine-producing neurons, but why these cells die is not entirely clear. Instead, research points to a complex interplay of genetic, environmental, and cellular factors.
Genetic Factors
For most people, Parkinson’s is not inherited in a straightforward manner. However, genetics do play a role. Certain rare mutations in genes such as LRRK2, PARK7, PINK1, PRKN, and SNCA significantly increase the risk of developing Parkinson’s. These mutations are more common in families with multiple affected members, though they represent a small percentage of overall cases.
Beyond rare mutations, there are genetic variations that slightly increase susceptibility when combined with environmental triggers. In other words, genes may open the door, but the environment often determines whether someone walks through it.
Environmental Triggers
Over the past few decades, researchers have uncovered links between Parkinson’s disease and environmental exposures. Long-term exposure to pesticides, herbicides, and certain industrial chemicals has been associated with an increased risk. Rural living, well water consumption, and farming—environments where such chemicals are more common—have also been connected to higher incidence rates.
On the other hand, interesting protective factors have been observed. People who smoke tobacco or drink caffeine appear to have a lower risk, though the reasons remain unclear and certainly do not suggest smoking as a preventative measure. Instead, these observations highlight the complex and sometimes surprising biology underlying the disease.
The Cellular Level: Protein Misfolding and Oxidative Stress
Inside the neurons of people with Parkinson’s, scientists often find abnormal clumps of protein called Lewy bodies. These clumps are primarily made up of a protein called alpha-synuclein, which in healthy cells has important functions. But when alpha-synuclein misfolds and aggregates, it becomes toxic, interfering with cell survival.
Additionally, oxidative stress—damage caused by unstable molecules called free radicals—contributes to the death of dopamine-producing neurons. Mitochondrial dysfunction, where the cell’s energy factories begin to fail, also plays a role in weakening neurons and making them more vulnerable.
Thus, Parkinson’s disease is not caused by one single factor but rather emerges from a storm of genetic predispositions, environmental exposures, and cellular breakdowns.
Symptoms: The Human Experience of Parkinson’s
When people think of Parkinson’s disease, they often picture the tremor—the characteristic shaking of the hands. While tremor is indeed a hallmark symptom, the reality of Parkinson’s is far broader and more complex. Symptoms unfold gradually and vary widely among individuals, affecting movement, speech, cognition, and mood.
Motor Symptoms
The motor (movement-related) symptoms are the most recognizable.
- Tremor: Usually begins in one hand or arm, often described as a “pill-rolling” motion between the thumb and forefinger. Tremor is most noticeable at rest and may lessen with purposeful movement.
- Bradykinesia (slowness of movement): This is perhaps the most disabling symptom. Simple tasks like buttoning a shirt, brushing teeth, or walking can take much longer than before. Movements become small and effortful.
- Rigidity: Muscles become stiff, limiting range of motion and causing discomfort. Rigidity can also contribute to a stooped posture.
- Postural instability: Balance becomes impaired, increasing the risk of falls.
These motor symptoms combine to make everyday activities challenging and can slowly strip away independence.
Non-Motor Symptoms
Less visible, but equally impactful, are the non-motor symptoms of Parkinson’s.
- Sleep disturbances: Insomnia, vivid dreams, and REM sleep behavior disorder (where people physically act out dreams) are common.
- Mood disorders: Depression, anxiety, and apathy often appear, sometimes even before motor symptoms.
- Cognitive changes: As the disease progresses, some individuals experience memory problems, difficulty concentrating, and even dementia.
- Autonomic dysfunction: Parkinson’s can affect automatic body functions, leading to constipation, low blood pressure, excessive sweating, or urinary problems.
- Loss of sense of smell: Many people notice reduced or lost ability to smell years before motor symptoms appear.
The combination of motor and non-motor symptoms makes Parkinson’s a whole-body disease, not just a movement disorder.
The Challenge of Diagnosis
Diagnosing Parkinson’s disease is not as straightforward as a blood test or brain scan. Instead, it is primarily a clinical diagnosis, made by a neurologist based on symptoms, medical history, and physical examination.
Doctors look for the cardinal motor symptoms: tremor, bradykinesia, rigidity, and postural instability. The presence of at least two of these, especially bradykinesia plus either tremor or rigidity, raises strong suspicion.
To support the diagnosis, doctors may also assess the patient’s response to Parkinson’s medications. A significant improvement with drugs like levodopa strongly suggests Parkinson’s disease.
Advanced imaging techniques, such as dopamine transporter (DaT) scans, can visualize dopamine activity in the brain and help differentiate Parkinson’s from other movement disorders. However, no single test can confirm the disease with absolute certainty.
Because symptoms often emerge gradually, early diagnosis can be difficult. Some people live for years with vague signs—slight stiffness, fatigue, or loss of smell—before the condition is recognized.
Treatment: Managing Parkinson’s with Science and Compassion
There is no cure for Parkinson’s disease yet, but treatment can significantly improve quality of life. Management involves a combination of medications, therapies, lifestyle adjustments, and sometimes surgical interventions. The goal is not only to relieve symptoms but also to maintain independence, dignity, and hope.
Medications
The cornerstone of Parkinson’s treatment is medication to restore or mimic dopamine.
- Levodopa (combined with carbidopa): The most effective drug, levodopa is converted into dopamine in the brain, improving movement. Carbidopa prevents levodopa from breaking down before reaching the brain, reducing side effects.
- Dopamine agonists: These drugs mimic dopamine’s effects and can be used alone in early stages or with levodopa later.
- MAO-B inhibitors and COMT inhibitors: These block enzymes that break down dopamine, prolonging its effects.
- Anticholinergics: Useful for tremor but less commonly used today due to cognitive side effects.
Over time, however, long-term levodopa use can lead to motor complications such as dyskinesias (involuntary movements) and “on-off” fluctuations, where symptoms suddenly worsen as the drug’s effect wears off.
Surgical Treatments
For patients with advanced Parkinson’s whose symptoms are not well controlled with medication, surgery may be an option.
- Deep Brain Stimulation (DBS): Electrodes are implanted into specific brain regions and connected to a pacemaker-like device in the chest. By sending electrical impulses, DBS can dramatically reduce motor symptoms and medication needs.
Supportive Therapies
Managing Parkinson’s is not just about medication or surgery—it also requires holistic support.
- Physical therapy helps maintain strength, balance, and mobility.
- Speech therapy addresses difficulties with speech and swallowing.
- Occupational therapy adapts daily activities and environments for safety and independence.
- Counseling and mental health support are crucial for addressing depression, anxiety, and emotional challenges.
Lifestyle and Wellness
Regular exercise is one of the most powerful non-drug interventions. Activities like walking, swimming, dancing, yoga, or tai chi improve mobility, balance, and even mood. Nutrition also matters; a diet rich in fruits, vegetables, whole grains, and lean proteins supports overall health and may ease some symptoms like constipation.
Support groups and community resources offer emotional connection, practical advice, and a sense of solidarity for both patients and caregivers.
Living with Parkinson’s: The Human Spirit
Parkinson’s disease changes lives, but it does not define them. Many people continue to live fulfilling, active, and joyful lives for decades after diagnosis. The journey is marked by resilience, adaptation, and the pursuit of meaning in the face of challenge.
Caregivers play an essential role, offering not only physical support but also love, patience, and understanding. Their journey, too, requires recognition and compassion, as caregiving is both rewarding and demanding.
Stories of individuals living with Parkinson’s remind us that health is not only about biology—it is about purpose, connection, and dignity. From advocates raising awareness to scientists seeking cures, the Parkinson’s community demonstrates remarkable strength and unity.
Research and Hope for the Future
Though a cure remains elusive, research into Parkinson’s disease is advancing rapidly. Scientists are exploring:
- Neuroprotective therapies aimed at slowing or halting neuron death.
- Stem cell therapies to replace lost dopamine-producing cells.
- Gene therapies to correct mutations or boost protective proteins.
- Immunotherapies targeting misfolded alpha-synuclein to prevent toxic buildup.
Advances in brain imaging, wearable devices, and artificial intelligence are also improving early detection and personalized care. Each step brings us closer to transforming Parkinson’s from a life-altering condition into a manageable one—and eventually, into a disease of the past.
Conclusion: Parkinson’s Disease as a Shared Journey
Parkinson’s disease is not just a neurological disorder; it is a profound human experience. It is the gradual loss of control over movements once taken for granted, but also the discovery of strength in vulnerability, resilience in adversity, and hope in science and community.
To understand Parkinson’s is to see both the microscopic world of misfolded proteins and the macroscopic world of human courage. It is to acknowledge suffering while also honoring perseverance. While the path is difficult, it is also illuminated by research, treatment advances, and the enduring human spirit.
Parkinson’s disease reminds us that health is not merely the absence of illness but the capacity to live meaningfully even in its presence. And as science marches forward, so too does the hope that one day, the story of Parkinson’s will end not with struggle, but with cure.