The human body is an extraordinary network of interacting systems that work in harmony to sustain life. From the beating of the heart to the regulation of body temperature, every process within us operates under a delicate balance. This internal stability is called homeostasis, a fundamental biological principle that ensures the body’s internal environment remains constant despite changes in the external world.
Homeostasis is vital because the cells that make up the human body require specific conditions to function optimally. A slight deviation from these conditions can lead to malfunction or even death. For instance, blood pH must stay within a narrow range, body temperature must be maintained around 37°C (98.6°F), and glucose levels in the blood must remain balanced to fuel cellular activity. The body continuously monitors and adjusts these variables through a complex network of feedback mechanisms involving the nervous, endocrine, and other physiological systems.
The concept of homeostasis is central to physiology and medicine because it explains how living organisms maintain internal stability, adapt to stress, and recover from disturbances. To understand life itself, one must understand homeostasis.
The Concept and Origin of Homeostasis
The term homeostasis originates from two Greek words: homeo, meaning “similar,” and stasis, meaning “standing still.” The concept was first proposed by the American physiologist Walter Cannon in the early 20th century, building on earlier work by the French scientist Claude Bernard, who introduced the idea of the “milieu intérieur” or internal environment.
Bernard recognized that for an organism to survive, its internal environment must remain constant even when the external environment changes. Cannon expanded this idea and coined the term homeostasis to describe the self-regulating processes that maintain physiological stability. He also emphasized that this regulation is dynamic rather than static; the body is constantly adjusting, not remaining perfectly still.
For example, body temperature fluctuates slightly throughout the day, and blood sugar levels rise after eating and fall during fasting. These variations are normal because the body continuously corrects them through feedback mechanisms that act like biological control systems.
Homeostasis is thus not about perfect constancy but about controlled equilibrium—where internal conditions are maintained within narrow, healthy limits through continuous adjustments.
The Principles of Homeostasis
At the heart of homeostasis lie several fundamental principles that define how the body monitors and responds to internal and external changes.
Every homeostatic control system has three essential components: a receptor, a control center, and an effector. The receptor detects a change or stimulus in the environment, such as a rise in temperature or a drop in blood sugar. This information is sent to the control center, usually located in the brain or endocrine glands, which compares the data against a set point—a desired value or range. If the condition deviates from this set point, the control center activates effectors, such as muscles or glands, to initiate a response that restores balance.
This process forms what is known as a feedback loop, and the most common type in biological systems is the negative feedback loop. In negative feedback, the response counteracts the initial change, returning the system to its normal state. For instance, if body temperature rises, mechanisms are triggered to cool the body down. Conversely, if temperature drops, heat-generating processes are activated.
A positive feedback loop, though less common, amplifies changes instead of reversing them. These are usually involved in processes that must reach a definite conclusion, such as blood clotting or childbirth. In these cases, the system accelerates a process until a specific goal is achieved, after which normal regulation resumes.
Temperature Regulation: Maintaining Thermal Balance
One of the most well-known examples of homeostasis is thermoregulation—the control of body temperature. Humans are endothermic organisms, meaning they generate and regulate their own heat internally. The optimal core temperature for human physiology is around 37°C, and deviations beyond a few degrees can impair enzyme activity and disrupt metabolic processes.
The hypothalamus, a small but vital region of the brain, serves as the body’s thermostat. It receives input from temperature receptors in the skin and internal organs. When body temperature rises, as in a hot environment or during intense exercise, the hypothalamus activates mechanisms to dissipate heat. Blood vessels near the skin surface dilate, allowing more blood to flow close to the skin and release heat. Sweat glands also produce sweat, which cools the body as it evaporates.
Conversely, when the body becomes too cold, the hypothalamus triggers heat-conserving responses. Blood vessels constrict to reduce heat loss, and shivering begins as muscles contract rapidly to generate heat. Behavioral responses, such as seeking warmth or adding clothing, complement these physiological adjustments.
Thermoregulation illustrates how multiple systems—the nervous, circulatory, and muscular—work together to maintain balance. It is also an example of how homeostasis extends beyond automatic internal reactions to include conscious behaviors that protect equilibrium.
Blood Glucose Regulation: Balancing Energy Supply
Glucose is the body’s primary energy source, and maintaining its concentration in the blood is critical for proper cellular function. The body achieves this through a finely tuned homeostatic mechanism controlled mainly by the endocrine system, particularly the pancreas.
After eating, blood glucose levels rise as carbohydrates are broken down into glucose and absorbed into the bloodstream. In response, the pancreas releases the hormone insulin, which facilitates the uptake of glucose by cells for energy production and storage as glycogen in the liver and muscles. As glucose levels decrease, insulin secretion declines.
During fasting or physical activity, when blood glucose levels drop, another hormone called glucagon is released by the pancreas. Glucagon stimulates the breakdown of glycogen back into glucose, releasing it into the bloodstream to maintain adequate energy supply.
This interplay between insulin and glucagon forms a classic negative feedback system that keeps blood glucose within a narrow range. When this regulation fails, disorders such as diabetes mellitus occur, leading to chronic high blood sugar levels that can damage organs and tissues over time.
Fluid and Electrolyte Balance
Water and electrolytes—ions such as sodium, potassium, and chloride—are essential for maintaining the body’s internal environment. They influence blood pressure, nerve conduction, muscle contraction, and cellular function. Homeostasis of fluids and electrolytes is achieved through interactions between the kidneys, endocrine glands, and circulatory system.
The kidneys play the central role in regulating fluid balance. They filter the blood, selectively reabsorbing water and electrolytes or excreting them in urine. This process is influenced by hormones such as antidiuretic hormone (ADH), which increases water reabsorption when the body is dehydrated, and aldosterone, which promotes sodium retention and potassium excretion.
When fluid levels are too high, ADH secretion decreases, resulting in increased urine output. Conversely, when dehydration occurs, the hypothalamus stimulates thirst and increases ADH release to conserve water. These mechanisms ensure that the composition and volume of body fluids remain within healthy limits despite variations in water intake or environmental conditions.
pH Regulation and Acid-Base Balance
The pH of the human body is another critical variable that must be carefully controlled. The normal blood pH range is approximately 7.35 to 7.45, which is slightly basic. Even minor deviations can disrupt enzyme function and metabolic reactions.
The body maintains pH homeostasis through three main systems: chemical buffers, respiratory control, and renal regulation.
Chemical buffers, such as the bicarbonate buffer system, act almost instantly to neutralize excess acids or bases. For example, when carbon dioxide levels rise in the blood, it reacts with water to form carbonic acid, which can dissociate into hydrogen ions and bicarbonate. The balance between these components helps resist sudden pH changes.
The respiratory system contributes to pH control by adjusting the rate of carbon dioxide removal. If blood becomes too acidic, breathing rate increases, expelling more CO₂ and reducing acidity. The kidneys provide long-term regulation by excreting hydrogen ions and reabsorbing bicarbonate as needed.
Together, these systems maintain acid-base balance, preventing conditions like acidosis or alkalosis, which can be life-threatening if uncorrected.
The Role of the Nervous and Endocrine Systems in Homeostasis
The nervous and endocrine systems serve as the primary regulators of homeostatic processes, functioning as the body’s communication networks.
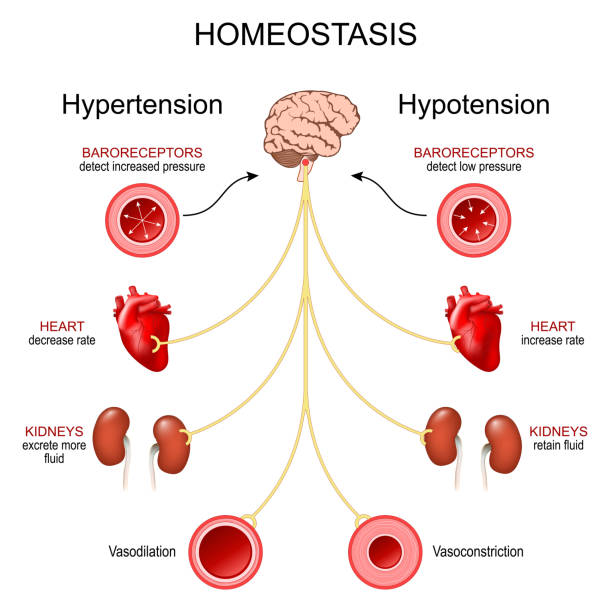
The nervous system provides rapid, short-term control through electrical signals. For example, when blood pressure drops, sensors called baroreceptors in the arteries detect the change and send signals to the brainstem. The brain responds by increasing heart rate and constricting blood vessels to restore normal pressure.
The endocrine system, by contrast, operates through hormones—chemical messengers that travel in the bloodstream and produce longer-lasting effects. Hormones regulate metabolism, growth, reproduction, and stress responses. For instance, the hypothalamus-pituitary-adrenal (HPA) axis manages stress by releasing cortisol, which mobilizes energy stores and suppresses nonessential functions until the body returns to normal conditions.
These two systems often work together. The hypothalamus, located at the base of the brain, serves as a critical link between them. It receives neural input about the body’s state and responds by adjusting hormonal output to maintain stability.
Cardiovascular and Respiratory Homeostasis
The cardiovascular and respiratory systems are tightly interconnected in maintaining oxygen delivery and carbon dioxide removal—both vital for homeostasis.
When the body requires more oxygen, such as during exercise, the respiratory rate increases to bring in more air, while the heart rate accelerates to deliver oxygen-rich blood to muscles. Sensors in the blood vessels detect changes in oxygen, carbon dioxide, and pH levels, sending feedback to the brain’s respiratory and cardiovascular centers. These centers coordinate the activity of the lungs and heart to meet the body’s metabolic demands.
If oxygen levels fall too low or carbon dioxide levels rise too high, the brain increases both the depth and rate of breathing to restore balance. This intricate coordination ensures that tissues receive adequate oxygen and that waste gases are efficiently expelled.
The Immune System and Homeostatic Defense
Homeostasis also extends to the immune system, which protects the body from infections, injuries, and internal disturbances. When pathogens invade, the immune system mounts a defense while ensuring that the response does not become excessive or destructive.
Inflammation, for example, is a controlled response that isolates damaged tissue and promotes healing. However, excessive inflammation can disrupt homeostasis, leading to autoimmune diseases or chronic conditions. Thus, immune regulation is another form of balance—activating defenses when needed and suppressing them when the threat has passed.
Cytokines, hormones, and neural signals interact to coordinate immune activity with other physiological systems. This integration ensures that energy is conserved for vital functions and that stress responses do not overwhelm immune regulation.
Homeostasis and Stress
Stress, whether physical or psychological, challenges homeostasis. When the body perceives a threat, the sympathetic nervous system triggers the “fight or flight” response. Heart rate and breathing accelerate, glucose is released for energy, and blood flow is redirected to essential organs.
While this acute stress response is adaptive, chronic stress can disrupt homeostasis. Prolonged elevation of stress hormones like cortisol can impair immune function, disturb metabolism, and contribute to diseases such as hypertension, diabetes, and depression.
Restoring balance after stress requires activation of the parasympathetic nervous system, which promotes rest, digestion, and recovery. The ability to adapt to stress and reestablish equilibrium is known as allostasis, a concept closely related to homeostasis but emphasizing the body’s capacity for dynamic adjustment under changing conditions.
Homeostatic Imbalance and Disease
When homeostatic mechanisms fail, the result is disease. Many disorders can be understood as disruptions of internal balance. For example, in diabetes, the inability to regulate blood glucose leads to chronic metabolic instability. In dehydration, fluid balance is lost, impairing circulation and cellular function. In heatstroke, thermoregulatory mechanisms are overwhelmed.
Aging also weakens homeostatic regulation. As organs lose efficiency and feedback responses slow, the body becomes less capable of maintaining equilibrium under stress. This decline contributes to the increased vulnerability to illness seen in older adults.
Understanding these imbalances provides insight into prevention and treatment. Medical therapies often aim to restore homeostasis, whether through insulin injections for diabetes, electrolyte replacement for dehydration, or temperature management for fever.
Cellular and Molecular Mechanisms of Homeostasis
Homeostasis begins at the cellular level. Each cell maintains its internal environment through processes such as membrane transport, energy metabolism, and signaling. The cell membrane plays a crucial role by controlling the movement of ions and molecules in and out of the cell. Ion channels and pumps regulate sodium, potassium, calcium, and other essential elements, ensuring proper electrical and chemical balance.
Molecular chaperones, enzymes, and genetic regulators also contribute to stability by repairing damage, maintaining protein structure, and adjusting gene expression in response to stress. When cells fail to maintain homeostasis, they may undergo apoptosis, or programmed cell death, to prevent harm to the organism as a whole.
Evolutionary Perspective of Homeostasis
Homeostasis is not unique to humans; it is a universal feature of life. From single-celled organisms to complex mammals, all living beings maintain internal balance. In unicellular organisms, homeostasis involves regulating ion concentrations and osmotic pressure, while in multicellular organisms, specialized organs and systems evolved to perform these functions.
The evolutionary advantage of homeostasis is clear—it allows organisms to survive in fluctuating environments. For example, warm-blooded animals can inhabit cold regions because they maintain internal temperature, while plants adjust water retention to survive droughts. This adaptability has been essential to the survival and diversification of life on Earth.
The Future of Homeostatic Research
Modern science continues to explore homeostasis through new technologies such as genomics, bioinformatics, and systems biology. Researchers are uncovering how genetic networks, molecular pathways, and environmental factors interact to sustain balance.
Advances in artificial intelligence and biomedical engineering are enabling precise monitoring of physiological variables through wearable devices and smart implants. These innovations may one day allow personalized medical systems that automatically detect and correct homeostatic disturbances before symptoms appear.
Moreover, the study of homeostatic plasticity in neuroscience is revealing how the brain maintains stable function despite constant changes in neural activity. Understanding these mechanisms may lead to breakthroughs in treating neurological disorders, mental health conditions, and age-related cognitive decline.
Conclusion
Homeostasis is the foundation of life—a continuous process through which the human body maintains internal stability amid external change. It governs every physiological function, from heartbeat and breathing to digestion and immunity. Through intricate feedback loops, the body monitors and corrects deviations, ensuring that temperature, pH, glucose, and countless other factors remain within narrow, life-sustaining limits.
When homeostasis is disrupted, disease arises; when it is restored, health returns. The study of homeostasis therefore bridges biology and medicine, linking cellular processes to the health of the entire organism.
Ultimately, homeostasis exemplifies the remarkable intelligence of life itself. It is a symphony of systems working together in perfect harmony, a dance of constant adjustment and renewal that defines what it means to be alive. Through understanding homeostasis, we not only learn how the human body functions but also gain insight into the delicate balance that sustains all living things on Earth.