The kidneys, two small organs shaped like beans, weigh just a few ounces each, yet they are responsible for one of the most important functions in the body: filtration. Situated at the lower back, one on either side of the spine, they quietly perform their tasks day and night, regulating a variety of vital processes without drawing attention to themselves. Despite their unobtrusive nature, the kidneys are crucial to our survival.
Kidneys filter blood, remove waste, and maintain the balance of essential bodily fluids, electrolytes, and toxins. They help regulate blood pressure, contribute to the formation of red blood cells, and even influence the body’s calcium and vitamin D metabolism. Without these organs functioning efficiently, life itself would not be possible.
In this article, we explore the critical role of the kidneys in the filtration process, breaking down how they work to maintain homeostasis in the body, protect against harmful substances, and contribute to overall health.
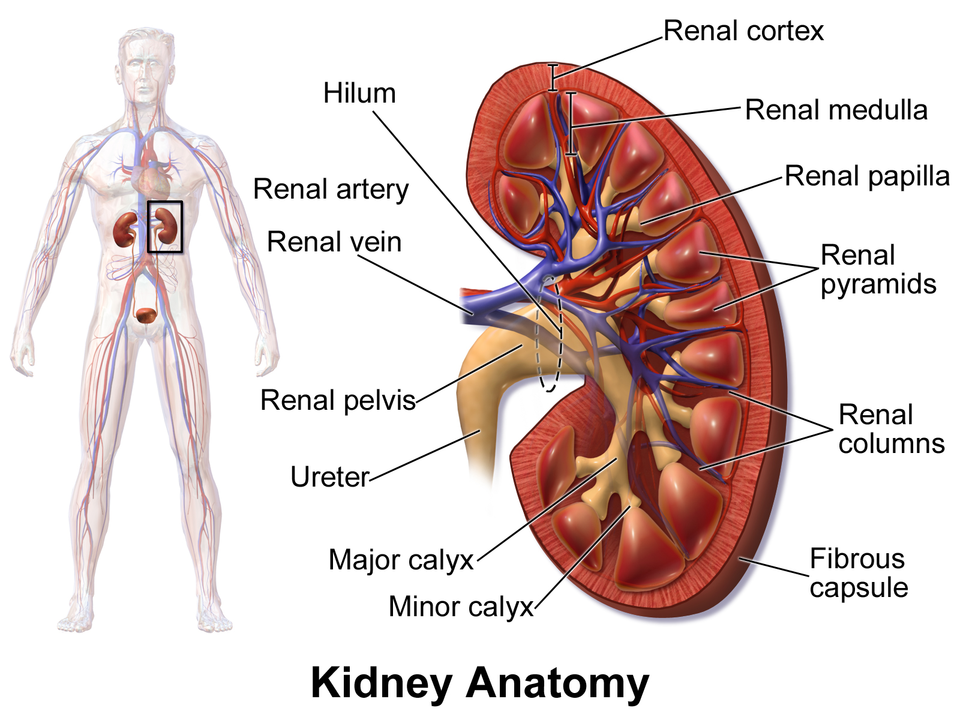
The Kidney’s Anatomy: A Marvel of Design
Before we dive into how the kidneys filter blood, it’s important to first understand their structure. The kidneys are made up of intricate networks of specialized cells and systems that work in harmony to perform their vital functions. The kidney is divided into several regions, each with a unique role in the filtration process.
At the core of each kidney is the nephron, the basic structural and functional unit. The nephron consists of a small cluster of blood vessels and a series of tubules. There are roughly one million nephrons in each kidney, collectively making up the functional powerhouse of the organ. The nephron’s key components include the glomerulus, the proximal convoluted tubule, the loop of Henle, the distal convoluted tubule, and the collecting duct.
The glomerulus, a network of capillaries, is the first place where blood enters the nephron. It’s in the glomerulus where filtration begins. From there, the filtered fluid passes through the rest of the nephron’s tubules, where essential substances are reabsorbed, and waste products are concentrated into urine.
But the kidneys’ job is not limited to filtration alone. They are also responsible for regulating the composition of the blood, balancing electrolytes like sodium and potassium, and managing the body’s fluid levels. The kidneys maintain the acid-base balance by filtering out hydrogen ions, helping to ensure that the blood’s pH remains within the optimal range for cellular function.
Filtration: The First Step in Kidney Function
The primary function of the kidneys is filtration. Blood enters the kidneys through the renal artery, which branches into smaller blood vessels and eventually reaches the glomeruli. At the glomerulus, blood is filtered under pressure through a specialized filtration barrier that allows only certain substances to pass through. This process is highly selective and designed to remove waste products while retaining vital nutrients.
The filtration process begins when blood flows into the afferent arteriole, which carries the blood to the glomerulus. Within the glomerulus, a high-pressure environment forces water and small molecules, such as glucose, salts, urea, and amino acids, through tiny holes in the walls of the capillaries. Larger molecules, like proteins and blood cells, are too large to pass through this barrier and remain in the bloodstream.
The result is the formation of glomerular filtrate—a fluid that is very similar to plasma but free of proteins and blood cells. This filtrate flows into the Bowman’s capsule, a cup-shaped structure that collects the filtered fluid. From here, the filtrate enters the various parts of the nephron for further processing.
Reabsorption: Keeping What the Body Needs
While filtration removes waste from the blood, it also removes substances that the body needs. Therefore, the kidneys must carefully reabsorb essential compounds to maintain the body’s balance.
The first place where reabsorption occurs is in the proximal convoluted tubule (PCT), which is a long, twisted tube located near the Bowman’s capsule. As the filtrate passes through the PCT, most of the water, glucose, amino acids, and electrolytes like sodium and potassium are reabsorbed into the bloodstream. This process occurs through both passive and active transport mechanisms. For instance, glucose and amino acids are actively transported across the walls of the tubule and into the surrounding capillaries, while water moves by osmosis, following the movement of sodium ions.
The amount of reabsorption that takes place is finely tuned to the body’s needs. If the body is dehydrated, more water will be reabsorbed to conserve fluid. If there is excess salt in the body, less sodium will be reabsorbed to eliminate the excess. The kidneys’ ability to adjust reabsorption rates is one of the key mechanisms that helps maintain fluid and electrolyte balance.
After the filtrate leaves the PCT, it enters the loop of Henle, a U-shaped structure that plays a crucial role in concentrating urine. The loop of Henle has two limbs: the descending limb, which is permeable to water, and the ascending limb, which is impermeable to water but actively transports sodium and chloride ions. This design creates a concentration gradient in the medulla of the kidney, enabling the kidneys to concentrate urine and conserve water when needed.
From the loop of Henle, the filtrate moves into the distal convoluted tubule (DCT), where further reabsorption of sodium, chloride, and calcium ions takes place. The DCT also plays a role in regulating the pH of the blood by secreting hydrogen ions into the filtrate. By adjusting the amount of hydrogen ions excreted, the kidneys can help maintain the body’s acid-base balance.
The last step of filtration processing occurs in the collecting duct, which is where the final concentration of urine occurs. Here, the hormone antidiuretic hormone (ADH) plays a crucial role. When the body is dehydrated, ADH signals the kidneys to reabsorb more water, resulting in more concentrated urine. Conversely, when the body is hydrated, ADH levels drop, leading to less water reabsorption and more diluted urine.
Secretion: Expelling Waste and Extra Substances
In addition to reabsorption, the kidneys also perform the important function of secretion. Secretion is the process by which certain substances are actively transported from the blood into the nephron for excretion in the urine. This allows the kidneys to remove substances that weren’t initially filtered out by the glomerulus but need to be eliminated from the body.
The proximal convoluted tubule, distal convoluted tubule, and collecting duct all contribute to secretion. Substances like hydrogen ions, potassium ions, ammonia, and certain drugs or toxins are actively secreted into the filtrate. This process is especially important in maintaining electrolyte balance and the body’s acid-base equilibrium.
For example, if the blood becomes too acidic, the kidneys can secrete hydrogen ions into the urine, thereby helping to neutralize the blood’s pH. Similarly, excess potassium ions, which are crucial for normal cell function, are actively secreted into the urine when their levels in the blood are elevated.
Regulation of Blood Pressure: A Secondary Role with Profound Impact
While the kidneys’ primary function is filtration, they also play a vital role in regulating blood pressure through a system known as the renin-angiotensin-aldosterone system (RAAS). Blood pressure regulation is essential for ensuring that blood is effectively pumped to all organs and tissues in the body.
When blood pressure drops, the kidneys release renin, an enzyme that triggers a cascade of reactions leading to the production of angiotensin II, a powerful vasoconstrictor. Angiotensin II causes blood vessels to constrict, increasing blood pressure. Additionally, it stimulates the release of aldosterone, a hormone that promotes sodium and water retention by the kidneys. This retention increases blood volume and further raises blood pressure.
The kidneys constantly monitor the body’s fluid balance and adjust blood pressure as needed to ensure that tissues receive an adequate blood supply. This function is critical for preventing complications like kidney failure or stroke, which can result from uncontrolled high or low blood pressure.
Excretion of Waste Products: The End of the Filtration Process
After all the reabsorption, secretion, and regulation processes have taken place, the remaining fluid, now known as urine, is ready to be excreted from the body. Urine consists primarily of water, along with waste products such as urea, creatinine, uric acid, and excess salts.
These waste products are byproducts of cellular metabolism and must be eliminated from the body to prevent toxicity. Urea, for example, is a waste product generated from the breakdown of proteins. If allowed to accumulate in the bloodstream, urea can be toxic. Therefore, the kidneys’ ability to filter out and excrete these waste products is essential for the maintenance of a healthy internal environment.
The urine flows from the collecting ducts into the renal pelvis, a funnel-shaped cavity at the center of the kidney. From there, it is transported to the bladder via the ureters, where it is stored until it is ready to be expelled from the body through the urethra.
The Kidney’s Role in Homeostasis
Beyond filtration, the kidneys are central to the maintenance of homeostasis—the body’s ability to maintain a stable internal environment despite external changes. Homeostasis encompasses a wide range of functions, including regulating fluid balance, electrolytes, acid-base balance, and blood pressure.
For example, if the body becomes dehydrated, the kidneys work to conserve water by reabsorbing as much as possible during filtration. If the body is overhydrated, the kidneys increase urine output to eliminate the excess water. Similarly, if sodium levels in the blood become too high, the kidneys excrete more sodium in the urine, and if potassium levels are too low, they conserve potassium by reducing urinary excretion.
In this way, the kidneys work tirelessly to ensure that the body’s internal conditions remain stable, allowing cells to function optimally.
The Consequences of Kidney Dysfunction
Given the vital roles the kidneys play in maintaining health, any dysfunction in these organs can have serious consequences. Kidney disease, which can arise from a variety of causes such as diabetes, high blood pressure, infections, or genetic conditions, can impair the kidneys’ ability to filter waste and regulate bodily functions.
When the kidneys fail to function properly, waste products can accumulate in the bloodstream, leading to symptoms such as swelling, fatigue, difficulty breathing, and confusion. Severe kidney dysfunction may necessitate treatments like dialysis, a process that artificially filters the blood, or a kidney transplant.
Preventing kidney damage involves managing underlying health conditions, staying hydrated, eating a balanced diet, and avoiding substances that can harm the kidneys, such as excessive salt and alcohol.
Conclusion: The Unsung Heroes of the Body
The kidneys are often taken for granted, functioning silently in the background to ensure that the body’s internal environment remains stable and healthy. Through the complex processes of filtration, reabsorption, secretion, and waste elimination, they help maintain balance and regulate essential bodily functions. From controlling blood pressure to removing toxins, the kidneys are vital to our survival.
As we continue to learn more about these remarkable organs, it becomes increasingly clear that their role in human health is as sophisticated as it is essential. Whether they are filtering the blood or contributing to homeostasis, the kidneys are unsung heroes in the body’s quest for balance.
In the end, the kidneys may be small in size, but their importance cannot be overstated. They are central to life itself. And perhaps, the
more we appreciate and understand their functions, the better equipped we will be to take care of them and ensure they continue working effectively for years to come.