Polycystic Ovary Syndrome—commonly abbreviated as PCOS—sounds like a complicated, almost cryptic phrase. And in many ways, it is. It’s a condition that has confounded scientists, frustrated doctors, and deeply impacted the lives of millions of women across the world. At first glance, it might appear to be just a hormonal disorder involving the ovaries, but PCOS is far more than that. It’s a systemic condition that can influence a woman’s metabolism, emotions, appearance, and fertility—sometimes all at once.
Despite being one of the most common endocrine disorders among women of reproductive age, PCOS remains widely misunderstood and often underdiagnosed. Its symptoms can vary drastically from person to person, making it a diagnostic challenge even for experienced healthcare professionals. And because the condition touches so many aspects of health—hormonal balance, insulin resistance, mental health, skin, weight, and fertility—treating it can require a complex, holistic approach.
But before diving into the strategies that can help manage and treat PCOS, it’s important to understand what it actually is, how it manifests, and why it can be so challenging to live with.
Behind the Name: Polycystic Ovary Syndrome
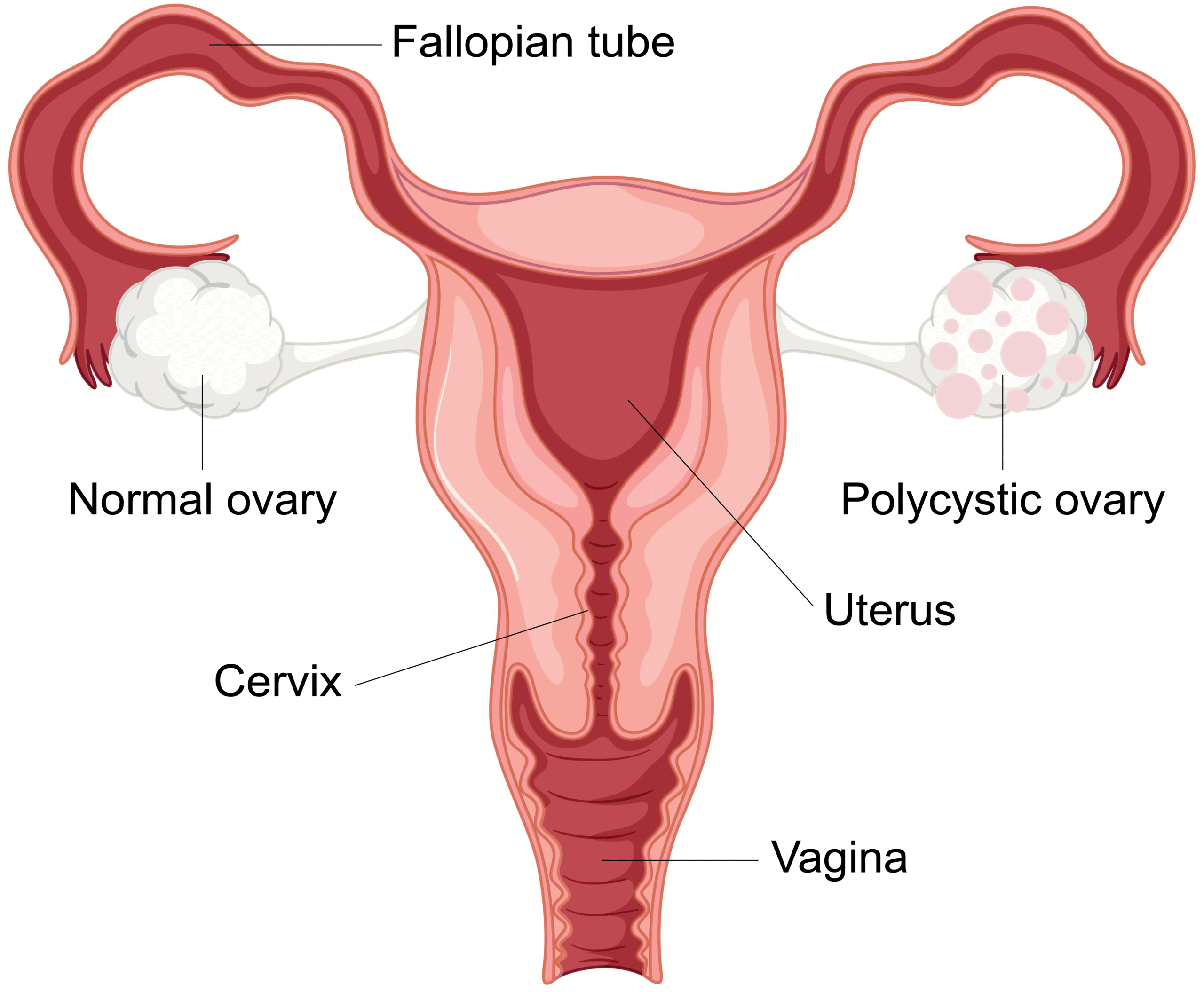
The name itself—Polycystic Ovary Syndrome—offers a clue, but not a full explanation. The term refers to the presence of multiple small cysts on the ovaries, which are often discovered during ultrasound exams. These are not dangerous or cancerous cysts, but rather immature follicles that have failed to properly ovulate.
However, the presence of cysts isn’t the defining feature for all women with PCOS. In fact, many women diagnosed with PCOS don’t have cystic ovaries at all, and some with cysts do not meet the criteria for PCOS. That’s why the name is considered somewhat misleading. The condition is defined less by the cysts themselves and more by a constellation of symptoms, including irregular periods, excess levels of androgens (male hormones), and signs of insulin resistance.
It is essentially a hormonal disorder rooted in the dysfunction of the endocrine system, but it doesn’t exist in isolation. PCOS interacts with the entire body’s network of hormones and organs, creating ripple effects that reach far beyond the ovaries.
The Hormonal Balancing Act Gone Awry
Hormones are the chemical messengers of the body, traveling through the bloodstream and telling organs and tissues what to do. In women with PCOS, this finely tuned symphony goes out of rhythm. Androgens—typically considered male hormones like testosterone—are often elevated. While all women produce androgens to some degree, those with PCOS tend to produce more than usual.
This hormonal imbalance leads to some of the hallmark symptoms of PCOS, such as excessive facial or body hair (a condition known as hirsutism), acne, and scalp hair thinning. At the same time, the hormonal seesaw affects ovulation. Ovulation might become irregular or stop altogether, leading to infrequent or absent menstrual periods and, in many cases, difficulty conceiving.
Another major player in the PCOS landscape is insulin, the hormone responsible for regulating blood sugar levels. A large proportion of women with PCOS are insulin resistant, meaning their bodies don’t respond to insulin effectively. In response, the pancreas pumps out even more insulin, creating a vicious cycle. Excess insulin can stimulate the ovaries to produce more androgens, which worsens the hormonal imbalance and perpetuates the symptoms.
The Many Faces of PCOS
PCOS doesn’t look the same in every woman. Some experience irregular or absent periods for years before seeking medical advice. Others struggle with unexplained weight gain, stubborn acne, or fertility challenges that eventually lead to a diagnosis. And then there are those for whom the emotional toll—mood swings, anxiety, or body image issues—is the most overwhelming part.
The condition is commonly divided into phenotypes, depending on which symptoms are most pronounced. Some women exhibit primarily reproductive issues; others may show metabolic disturbances, such as prediabetes or high cholesterol. Still, others may be lean and have regular cycles but suffer from high androgen levels or polycystic ovaries.
This variability makes PCOS a deeply personal condition. It also means that no two treatment plans should look exactly alike. The same condition that leaves one woman battling weight gain might leave another lean but infertile. PCOS is, in a very real sense, a shape-shifter.
The Emotional and Psychological Landscape
While PCOS is often discussed in terms of physical symptoms, its psychological impact deserves equal attention. Many women report feelings of frustration, confusion, and isolation following a diagnosis. For those trying to conceive, the uncertainty surrounding ovulation and fertility can be emotionally wrenching.
Depression and anxiety are significantly more common in women with PCOS than in the general population. This isn’t surprising when you consider the constant stress of managing irregular cycles, hormonal fluctuations, body image concerns, and the potential for long-term health complications. The condition often creates a feeling of being “out of control” of one’s own body, and that can erode self-esteem over time.
It’s critical to acknowledge this psychological dimension and treat it with the same seriousness as any physical symptom. Therapy, counseling, and support groups can play an essential role in the healing process.
How PCOS Affects Fertility—and What Can Be Done
One of the most emotionally charged aspects of PCOS is its impact on fertility. Ovulation is the cornerstone of natural conception, and when ovulation becomes infrequent or unpredictable, conceiving can become a long and emotionally draining journey.
However, PCOS-related infertility is not a closed door—it’s a door that may just take a bit more effort to unlock. With the right treatment and support, many women with PCOS go on to have healthy pregnancies. Sometimes, lifestyle changes alone can restore ovulation. In other cases, medication may be required to stimulate egg release or regulate cycles.
It’s worth noting that some women with PCOS are actually at a higher risk for multiple births when using fertility treatments, because more than one egg may be stimulated at a time. As with many aspects of PCOS, individualized care is key.
Treating PCOS: A Multifaceted Approach
Treating PCOS isn’t about finding a magic pill—it’s about building a toolkit. Because the syndrome manifests differently in every woman, treatment must be tailored to the individual. The goals might include regulating periods, managing symptoms like acne and hirsutism, supporting fertility, improving insulin sensitivity, or reducing the risk of long-term complications such as diabetes and cardiovascular disease.
One of the most powerful tools in managing PCOS is lifestyle change. Nutrition and physical activity can have a dramatic impact on hormone levels, insulin sensitivity, and overall metabolic health. This doesn’t mean adopting a restrictive or punishing approach to food and exercise. Instead, it means cultivating sustainable, nourishing habits that support the body’s natural rhythms.
In some cases, medications are needed to support or enhance these efforts. Birth control pills are commonly prescribed to regulate menstrual cycles and lower androgen levels. For women trying to conceive, medications like Clomid or letrozole can help induce ovulation. And when insulin resistance is a concern, metformin—a drug typically used for diabetes—can help regulate blood sugar and may even assist with weight management and ovulation.
Alternative therapies such as acupuncture, herbal medicine, and mindfulness practices are also gaining popularity in PCOS treatment. While the scientific evidence for some of these is still emerging, many women report meaningful relief from integrating holistic practices into their care plans.
The Long-Term Health Implications
PCOS doesn’t just affect the present—it can also influence future health in profound ways. Women with PCOS have a higher risk of developing type 2 diabetes, high blood pressure, elevated cholesterol, and heart disease. The constant hormonal imbalances can also increase the risk of endometrial cancer, particularly in those with prolonged, irregular menstrual cycles.
This makes long-term monitoring essential. Regular blood sugar screenings, cholesterol checks, and pelvic ultrasounds can help catch problems early. But perhaps even more important is the cultivation of daily habits that support cardiovascular and metabolic health.
It’s not just about avoiding disease—it’s about thriving in spite of a diagnosis.
The Power of Support and Advocacy
One of the most important aspects of navigating PCOS is realizing that you’re not alone. Because it’s so common—affecting an estimated 1 in 10 women—there’s a vast network of individuals, groups, and organizations working to raise awareness, support research, and offer community.
Support groups, whether in person or online, can provide a lifeline for those feeling isolated or overwhelmed. Talking with others who understand the struggle can offer not just emotional relief but practical advice—from recipes that support insulin sensitivity to tips for managing mood swings.
In recent years, PCOS has begun to gain more attention from the medical community, thanks in part to the advocacy of patients and healthcare professionals alike. But there is still a long way to go. Many women report feeling dismissed or misunderstood by doctors, especially in the early stages of their symptoms. That’s why continuing to educate both patients and providers is so crucial.
Hope on the Horizon: Research and Innovation
The scientific community is hard at work unraveling the mysteries of PCOS. New research is uncovering the genetic factors behind the condition, exploring the gut microbiome’s role in hormonal health, and developing novel therapies that could offer more targeted treatment with fewer side effects.
Some of the most exciting developments include non-hormonal medications that improve insulin sensitivity, advances in in-vitro fertilization techniques for women with PCOS-related infertility, and deeper studies into how nutrition and stress reduction can modulate hormone levels naturally.
As the understanding of PCOS becomes more nuanced, so too will the strategies for managing it—offering more personalized, compassionate care for future generations of women.
Living Beyond the Diagnosis
Receiving a diagnosis of PCOS can be daunting. It often brings more questions than answers and demands a level of self-awareness and lifestyle management that can feel overwhelming. But it can also be a call to deeper self-care, a chance to get to know your body more intimately, and an opportunity to build a healthier, more empowered life.
Women with PCOS are not broken. They are navigating a complex, often misunderstood condition that demands both medical insight and personal resilience. With the right knowledge, support, and care, it’s entirely possible not just to manage PCOS—but to thrive with it.