Bones are the silent scaffolding of our lives. They carry us from place to place, protect our vital organs, and give shape to everything from our smiles to our stride. Yet, for many women over 40, bones are also the part of the body most often forgotten—until a fracture reminds them, painfully and unforgettably, that bone health is not a luxury but a lifelong necessity.
For women, the stakes are especially high. By the time most reach their mid-forties, bone density begins to decline at an accelerated rate, largely due to hormonal shifts. Menopause, that inevitable biological transition, often marks the tipping point between strong bones and increased fragility. But bone health isn’t just about menopause, or even aging. It’s about habits, history, and how you care for your body today.
Understanding your bones—and how to keep them healthy beyond 40—is not just about preventing osteoporosis. It’s about investing in the quality of life for decades to come.
The Architecture of Bone: What’s Happening Beneath the Surface
Bones may seem solid and unchanging, but they’re actually dynamic living tissues. From childhood through young adulthood, your skeleton is constantly building itself, increasing in size and density. This process, called bone remodeling, involves two opposing forces: osteoblasts, which build new bone, and osteoclasts, which break down old bone.
In your twenties and early thirties, this cycle maintains a relatively even balance. Bone mass peaks somewhere around age 30, meaning that’s the age when your bones are at their most dense. After that, the breakdown process begins to slightly outpace the rebuilding, and over time, this subtle shift becomes more pronounced.
For women, the process takes a dramatic turn around menopause. Estrogen, the hormone that helps regulate the activity of bone-building cells, plummets, triggering a rapid loss in bone density. In the first five to ten years after menopause, women can lose up to 20% of their bone mass. And the effects aren’t just about numbers on a scan—they’re about falls, fractures, and freedom.
The Hidden Crisis: Osteoporosis and Its Consequences
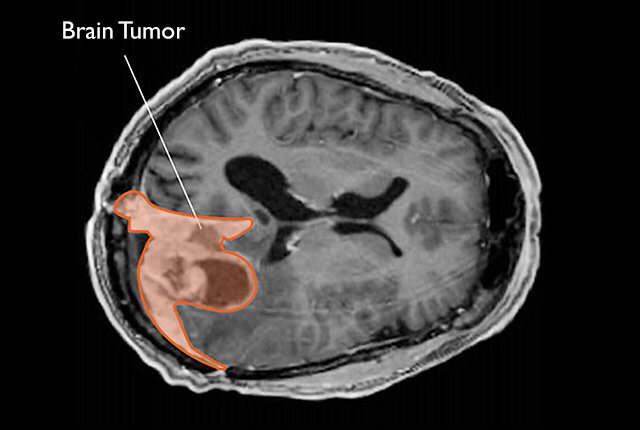
Osteoporosis, often called “the silent disease,” occurs when bones become so porous and fragile that even a minor bump or fall can cause a break. Hips, wrists, and spines are the most commonly affected areas, and the consequences can be life-altering.
A hip fracture in a 75-year-old woman isn’t just a broken bone; it can mean months in bed, loss of independence, and even increased mortality risk. Vertebral fractures can lead to chronic pain, a stooped posture, and difficulty breathing. Wrist fractures may seem minor but can compromise daily function and lead to long-term weakness.
The tragedy is that many of these fractures are preventable. Yet millions of women go undiagnosed and untreated until it’s too late. The reason? Bone loss is painless—until it isn’t.
Hormones and Bone Loss: The Estrogen Equation
Estrogen plays a vital role in keeping bones dense and strong. It inhibits bone resorption, the process by which bone is broken down and its minerals released into the bloodstream. When estrogen levels fall after menopause, bone resorption speeds up, and the body can’t replace lost bone quickly enough.
This estrogen-bone connection explains why women are disproportionately affected by osteoporosis compared to men. It also underscores why hormone-related conditions, like early menopause or removal of ovaries, can dramatically increase fracture risk if bone health isn’t addressed proactively.
But estrogen isn’t acting alone. Parathyroid hormone, calcitonin, vitamin D, and other hormones are part of the bone health orchestra. If one instrument is off-key—say, if you’re deficient in vitamin D—bone formation suffers. It’s a delicate symphony, and maintaining harmony becomes especially crucial after 40.
Calcium and Vitamin D: More Than Just Supplements
When people think of bone health, they usually think calcium. And rightly so—calcium is the main mineral found in bones. But its partner-in-crime, vitamin D, often gets less attention. Without vitamin D, your body can’t absorb calcium properly, no matter how much of it you take in.
After 40, many women become deficient in both. Dietary habits may change, sun exposure decreases (especially if you’re using sunscreen diligently, as you should), and the body’s ability to produce vitamin D declines with age.
But the answer isn’t simply to load up on calcium pills. Excess calcium without adequate magnesium and vitamin K2 can actually lead to calcification in arteries and soft tissues. It’s about balance and absorption, not just consumption.
Natural sources—leafy greens, fortified plant milks, fish like sardines and salmon, mushrooms, and egg yolks—are preferable when possible. But for many women, especially those in colder climates or with dietary restrictions, supplementation is necessary. The key is to take supplements as part of a larger strategy, not a magic fix.
The Movement Connection: Exercise and Bone Density
Your skeleton isn’t static; it responds to stress—specifically the kind of mechanical stress created by movement. Weight-bearing exercises, like walking, dancing, and hiking, stimulate bone-building cells by compressing the skeleton. Resistance training, such as lifting weights or doing Pilates, adds further incentive for your body to lay down more bone.
But not all exercise is equal. Swimming and cycling, while excellent for cardiovascular health, are not weight-bearing and do little for bone density. Yoga and tai chi, on the other hand, may not build bone directly but improve balance and flexibility, reducing the risk of falls.
Starting or continuing an exercise routine after 40 is one of the best gifts you can give your bones. It’s never too late. Even women in their 70s and 80s can increase bone strength and reduce fall risk with consistent, targeted movement.
The Food Factor: Eating for Bone Strength
Beyond calcium and vitamin D, your bones crave a rainbow of nutrients. Magnesium helps with calcium absorption and bone structure. Vitamin K2 helps shuttle calcium into bones and out of arteries. Zinc, manganese, and boron play lesser-known but equally important roles.
Protein, too, is vital. Despite outdated myths, protein doesn’t “leach calcium” from bones—in fact, low protein diets are associated with poorer bone health. Bones are about one-third protein by mass, and collagen—a protein—is the foundation upon which minerals are deposited.
What does this mean in the kitchen? Aim for colorful, whole-food meals that include leafy greens, nuts and seeds, legumes, fatty fish, fermented foods, and dairy or its fortified plant-based counterparts. Avoid excessive caffeine, alcohol, and sodium, which can accelerate calcium loss.
And perhaps most importantly: eat enough. Restrictive diets and chronic dieting—still far too common among women over 40—can lead to bone loss. Bones need fuel. So does the rest of you.
Genetics and the Bone Blueprint
Like eye color or height, your bone density has a genetic component. If your mother or grandmother had osteoporosis or suffered hip fractures, your risk increases. Certain ethnic backgrounds—especially Caucasian and Asian women—are at higher risk.
But genetics are not destiny. They’re a blueprint, not a sentence. Lifestyle still has a powerful impact, and even those with strong genetic predispositions can often delay or prevent fractures with the right habits.
Knowing your family history is crucial, though. It can inform when you should get a bone density scan (DXA scan) and help you and your doctor assess your risk more accurately.
Testing and Monitoring: What You Don’t Know Can Hurt You
The gold standard for assessing bone density is a DXA scan (dual-energy x-ray absorptiometry), which measures bone mineral density at the hip and spine. It’s quick, non-invasive, and relatively low-cost, but underutilized.
Current guidelines recommend that all women get a baseline scan at age 65, or earlier if they have risk factors such as early menopause, a family history of osteoporosis, smoking, steroid use, or certain medical conditions like rheumatoid arthritis or celiac disease.
But many women fall through the cracks. They don’t get scanned until after their first fracture—when prevention has already failed. The good news is that early detection can lead to early action, whether through lifestyle changes, supplements, or medication.
Bone turnover markers, urine tests, and blood calcium levels can also provide information, though they’re used less frequently. The important thing is to stay curious and proactive. Your bones aren’t going to shout for help—you’ll have to go looking.
Medications: Tools, Not Cures
For women at high risk of fracture, especially those already diagnosed with osteoporosis, medications can be lifesaving. Bisphosphonates, denosumab, hormone replacement therapy, and newer agents like romosozumab or parathyroid hormone analogs can all help maintain or increase bone density.
But these medications are not without risks. Some carry side effects like gastrointestinal issues, jaw osteonecrosis, or unusual fractures if taken for too long. Others, like hormone therapy, must be weighed carefully depending on a woman’s health history.
Still, for the right person, at the right time, these medications can dramatically reduce fracture risk and even reverse bone loss. They’re not a substitute for lifestyle changes, but they are powerful tools in a comprehensive approach.
The Emotional Weight of Fragility
There’s a psychological side to bone health that is often overlooked. A woman who suffers a fracture may not just feel pain—she may feel fear, vulnerability, even shame. The idea that her body has betrayed her, that she’s aging, that she’s breakable now in ways she wasn’t before—these are heavy burdens.
But bone strength is not just about avoiding injury. It’s about freedom: the freedom to walk without worry, to carry groceries without pain, to travel, garden, dance, and live on your own terms. Strong bones mean a strong life.
Women over 40 are often caretakers, professionals, parents, and community leaders. They pour energy into others. But tending to your own skeleton—quite literally the structure that holds you up—is not selfish. It’s essential.
Bone Wisdom: Aging with Grace and Strength
Growing older doesn’t mean growing weaker. In fact, midlife and beyond can be a time of incredible empowerment—physically, mentally, and spiritually. But it requires a shift in mindset. You are not the same woman you were at 25, and that’s not a loss—it’s an evolution.
Bone health is part of that evolution. It’s a reflection of your inner stability, your resilience, your grounding. And the choices you make in your 40s and 50s—about what you eat, how you move, how much sunlight you catch, and how you care for yourself—will ripple into the decades ahead.
So stand tall, literally and metaphorically. Embrace strength as a daily practice, not just a physical goal. Your bones are listening.