Menopause. The word itself can feel like a final act, a last curtain call on the stage of womanhood. But if you think menopause is a single moment in time—like a birthday or a light switch—you’re not alone. The truth, however, is far more complex and infinitely more interesting. Menopause isn’t a sudden change; it’s the culmination of a hormonal evolution that begins long before periods stop for good.
That winding, sometimes rocky road leading up to menopause is called perimenopause. And while menopause is often the headline, perimenopause is the real story. It’s the long, dramatic buildup—the unexpected plot twists, subtle shifts, and, yes, the occasional fire-breathing dragon in the form of a hot flash.
Understanding the difference between perimenopause and menopause isn’t just a matter of semantics. It can change how you see your body, your health, and this powerful midlife metamorphosis. This article dives deep into both phases, exploring what separates them, how they overlap, and what every woman should know to navigate this transformative chapter with knowledge, compassion, and perhaps even a bit of humor.
Defining Perimenopause: The Long Hello to Goodbye
Perimenopause means “around menopause,” and that’s exactly what it is. It’s the transitional phase that typically begins in a woman’s 40s, though for some, it can start as early as the mid-30s. It’s a biological prelude, where hormones—especially estrogen and progesterone—begin to waver and fluctuate like a violin warming up before a symphony.
This is the time when the ovaries, once reliable sources of monthly cycles, begin to show signs of slowing down. But they don’t go quietly. In perimenopause, the ovaries often become erratic, releasing hormones in unpredictable doses. Some months they might act like nothing’s changed at all; others, they flood the body or go silent altogether.
During perimenopause, the menstrual cycle becomes irregular. Periods might come closer together, farther apart, heavier, lighter, longer, shorter—or disappear entirely, only to return with a vengeance. It’s a hormonal rollercoaster, and not everyone rides it the same way.
Symptoms emerge subtly at first—maybe a harder time falling asleep, or a sudden hot flash that feels like your skin has been sun-kissed from the inside out. Mood swings, anxiety, brain fog, and fatigue might sneak in, often mistaken for stress, burnout, or simply “getting older.” But beneath the surface, perimenopause is underway, reshaping the body’s endocrine landscape.
The Menopause Moment: One Year, No Periods
Menopause itself is not a process. It’s a single point in time—a milestone. Technically, it’s defined as 12 consecutive months without a menstrual period, and it marks the official end of a woman’s reproductive years.
There’s no lab test, no scan, and no magic number that announces, “You are now menopausal!” Only time can confirm it. Once those 12 months have passed without menstruation and there’s no other medical explanation for the pause, menopause has arrived.
But here’s where things get tricky. By the time menopause officially occurs, many women have already been experiencing perimenopausal symptoms for years. And the symptoms don’t always stop when menopause begins. In fact, for many, the challenges intensify or take on new forms.
Hot flashes, night sweats, and sleep disturbances may persist for months or years after menopause. Vaginal dryness, thinning hair, joint pain, memory lapses—these too can linger. Menopause is not the end of symptoms; it’s just the end of periods.
Hormonal Shifts: The Inner Tectonic Plates
The key to understanding the difference between perimenopause and menopause lies in hormones. During a woman’s reproductive years, estrogen and progesterone follow a predictable ebb and flow, orchestrating the menstrual cycle with almost clockwork precision. But in perimenopause, this harmony becomes dissonant.
Estrogen, the body’s master multitasker, is responsible for regulating periods, maintaining bone density, keeping the vagina lubricated, and even influencing mood and cognition. As estrogen levels begin to fluctuate wildly in perimenopause, so too do the systems it regulates.
Progesterone, which helps prepare the body for pregnancy and balances the effects of estrogen, also begins to decline. This hormonal drop can lead to heavier or irregular periods, since progesterone plays a key role in controlling the menstrual lining.
By the time menopause is reached, estrogen and progesterone levels have fallen to consistently low levels. The fluctuations are gone—but so is the hormonal support that the body had grown used to for decades. This absence can have widespread effects, influencing everything from cardiovascular health to skin elasticity.
Emotional Terrain: The Mind-Body Storm
Hormones don’t just influence physical processes; they play a huge role in mood, cognition, and emotional regulation. That’s why the emotional symptoms of perimenopause and menopause can be just as significant—if not more so—than the physical ones.
During perimenopause, mood swings can feel like a return to adolescence. One minute you’re laughing; the next, you’re inexplicably irritated, anxious, or in tears. Many women describe it as an emotional fog, where everything feels slightly “off.”
Insomnia is another emotional wildcard. Sleep becomes elusive, thanks to fluctuating hormones disrupting the body’s natural circadian rhythms. Night sweats can cause sudden wake-ups, while anxiety can keep the mind churning long after the lights are out.
In menopause, emotional symptoms may persist, but they often stabilize over time. The hormonal chaos of perimenopause gives way to a new, lower hormonal baseline. It’s not about wild swings anymore—it’s about adaptation to a new normal. Some women feel relief during menopause; others find it more difficult.
The good news? With awareness, support, and sometimes treatment, these symptoms can be managed. Understanding that what you’re feeling is not “just in your head” can be incredibly validating—and empowering.
The Body Speaks: Signs You Can’t Ignore
In both perimenopause and menopause, the body speaks in signs and signals. Some are loud and unmistakable; others are whispers. But together, they tell a story.
During perimenopause, hot flashes might erupt like spontaneous internal combustion. Night sweats leave sheets soaked and sleep interrupted. Weight gain—especially around the midsection—becomes more common, even without changes in diet or activity.
Hair may thin; skin may dry. Libido can wane, and vaginal dryness can make sex uncomfortable. These changes can be distressing, especially when they arrive without warning or seem to contradict everything you thought you knew about your body.
Menopause continues this conversation but in a different tone. The absence of estrogen can lead to more profound changes: bones may begin to lose density, increasing the risk of osteoporosis. The skin may lose collagen, becoming thinner and more prone to wrinkles. The urinary tract becomes more sensitive, leading to an increase in infections or urgency.
But menopause doesn’t mean resignation. These changes are not a punishment—they’re part of the body’s transition. And with awareness comes the ability to respond, adapt, and thrive.
Diagnosis and Testing: Knowing Where You Stand
One of the most frustrating aspects of this life stage is its diagnostic ambiguity. Perimenopause can’t be pinpointed with a single blood test because hormones are in constant flux. A woman might have high estrogen one day and low the next. That’s why symptoms—rather than lab results—often offer the clearest window into what’s going on.
Doctors may use FSH (follicle-stimulating hormone) levels as a general indicator. During perimenopause, FSH may begin to rise as the ovaries respond less effectively. By menopause, it is typically elevated and remains so. But again, FSH is not definitive on its own.
What matters most is the pattern of changes: the irregular cycles, the hot flashes, the shifting sleep patterns, and mood changes. A thorough medical history, symptom tracking, and open conversations with a healthcare provider are key to understanding your place in the menopause journey.
Treatment Options: From Hormones to Holistic Approaches
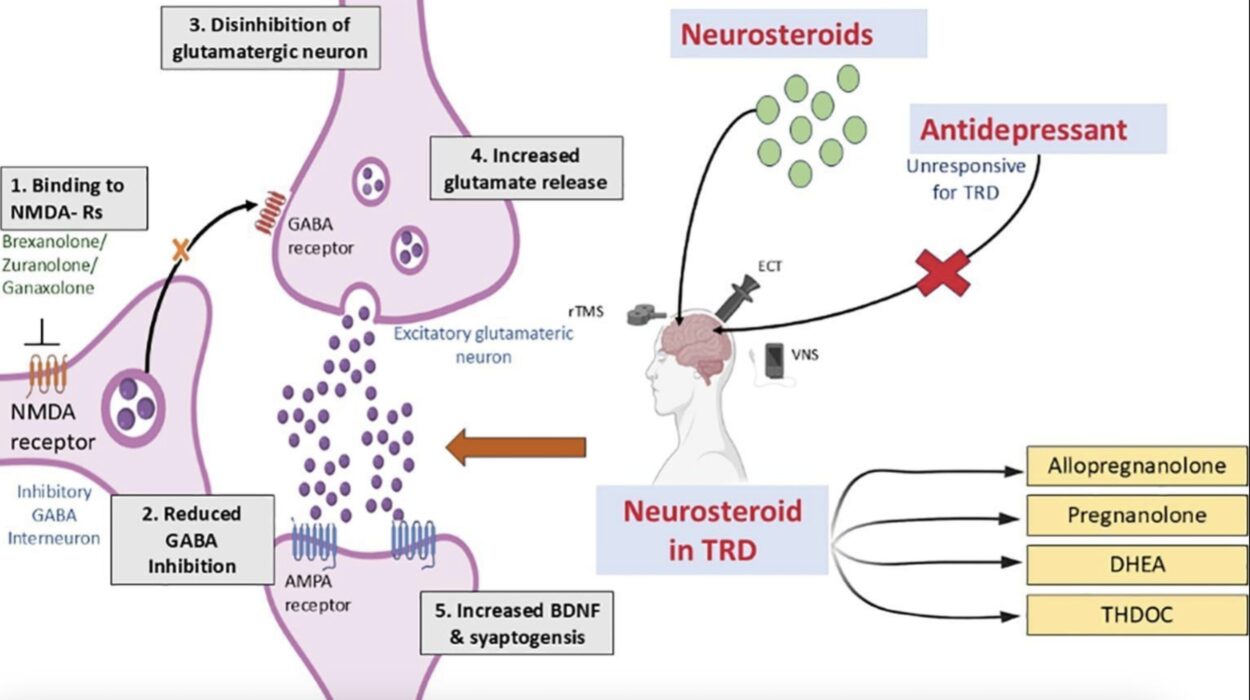
For those who struggle with severe symptoms, help is available. Hormone replacement therapy (HRT), once controversial, is now considered safe and effective for many women when started around the time of menopause. It can relieve hot flashes, prevent bone loss, and ease vaginal dryness.
But HRT isn’t for everyone, and not everyone wants it. Fortunately, there are other options. Antidepressants can help with mood swings and hot flashes. Sleep aids can offer temporary relief for insomnia. Vaginal estrogen creams can improve intimacy and urinary health without systemic effects.
Holistic approaches also shine during this phase. Nutrition plays a critical role: diets rich in calcium, magnesium, and phytoestrogens (like flaxseed and soy) can ease some symptoms. Exercise improves mood, strengthens bones, and supports heart health. Mind-body practices like yoga, meditation, and acupuncture offer additional tools for managing stress, sleep, and emotional well-being.
The goal is not to “fix” menopause—it’s to support the body and mind through the transition with compassion, strategy, and sometimes a bit of trial and error.
Cultural Narratives: From Shame to Strength
In many cultures, menopause has long been shrouded in silence. It’s been treated as an ending, a loss of fertility, femininity, and youth. Women have been taught to endure it quietly, to tuck away the symptoms and carry on.
But the tide is turning. A new generation is reclaiming the menopause narrative, demanding visibility, support, and science-based care. Menopause is being reframed not as a decline, but as an initiation—a passage into wisdom, power, and freedom from the monthly cycles that once dictated life.
Perimenopause, too, is stepping into the spotlight. No longer dismissed as a vague prelude, it is being recognized as a significant, often turbulent, and deeply personal experience. The more we talk about it, the more we can normalize the conversation, support one another, and create a culture that honors every stage of a woman’s life.
Conclusion: The Power of Knowing
So, what’s the difference between perimenopause and menopause? Perimenopause is the journey—sometimes winding, often surprising, and rarely linear. Menopause is the milestone—a pause that marks the end of menstruation and the beginning of a new hormonal chapter.
Together, they form a continuum, not a split. Understanding where you are on that continuum can be life-changing. It empowers you to make informed choices about your health, seek support when needed, and advocate for your body with clarity and confidence.
This isn’t just biology—it’s biography. It’s your story, written in hormones, symptoms, and resilience. Whether you’re at the beginning of perimenopause, moving through menopause, or well beyond it, your experience matters. And knowledge is your greatest ally.
You are not vanishing. You are evolving.